Clostridioides difficile, or C. diff, is a bacterium greatly impacting healthcare, causing over half a million infections, 15,000 deaths, and costing health care facilities $1.5 billion each year.1,2 This being C. diff Awareness Month, let’s take the opportunity to learn a bit more about this deadly pathogen, its impact, and what the future may bring.
History and Etiology
Discovered in 1935, Clostridioides difficile was first isolated and cultured by Hall and O’Toole. Proving to be a difficult process, this earned the microorganism its name difficile, meaning “difficult” in French. Although it was identified in the early 1900s, it wasn’t until 43 years later in 1978 that a connection was made between “the bug” — C. difficile, and what was then referred to as antibiotic-associated diarrhea by Dr. John Bartlett.3 From that point forward, efforts have been made through continued research, improved preventive measures, and advanced treatment methods to combat C. diff infections.
C. diff infections have a classic presentation with frequent watery loose stools — as many as 10–15 times a day — that carry a distinct foul odor. Although anyone can become infected with C. diff, certain individuals are at a higher risk. Highly susceptible persons include the elderly, people with serious underlying illness, or those taking or recently (within 30 days) completed an extended regimen of antibiotics. Antibiotic use is the leading risk factor for C. diff infections.4 Although we are learning more about community acquired incidence, most identified cases are healthcare-associated. C. diff is highly transmissible and has been shown to spread via healthcare workers hands which can pick up the pathogen from contaminated surfaces and medical equipment.5 Spores are also extremely resilient, surviving on surfaces for prolonged periods — up to 5 months, and are resistant to hand sanitizer and many disinfectants.6 For these reasons, C. diff continues to be the most common of all healthcare-associated infections (HAIs) and was labeled an urgent threat by the Centers for Disease Control and Prevention (CDC) in 2019.7
Pandemic Impact on HAI Rates
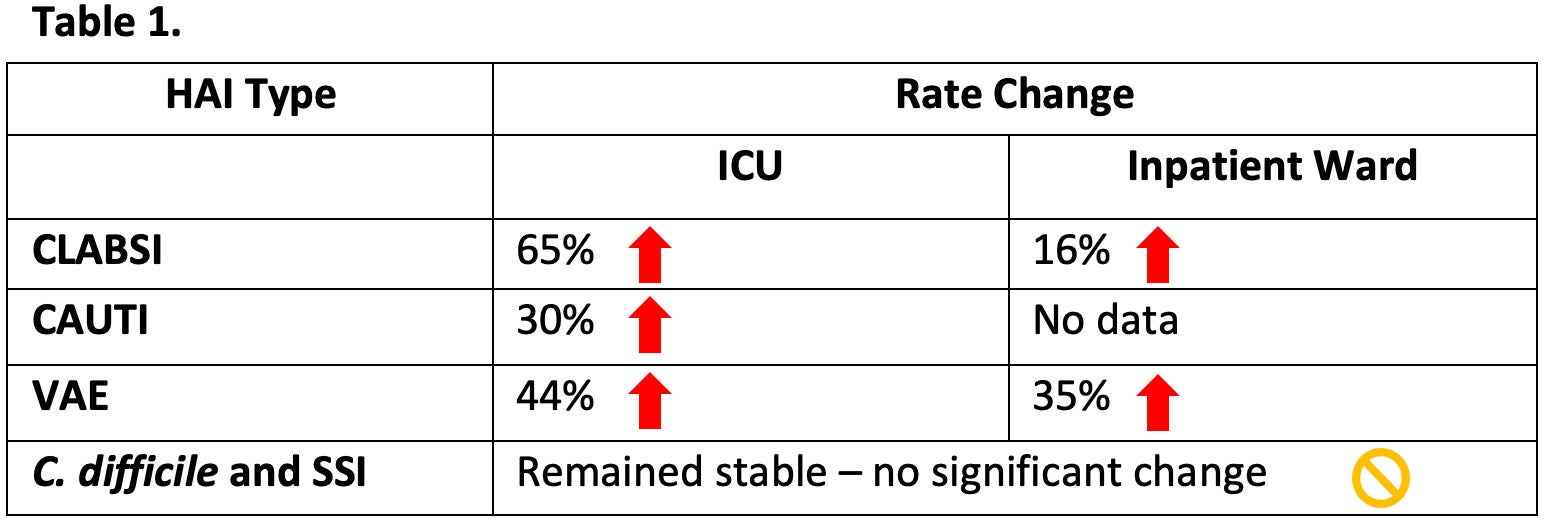
As the COVID-19 pandemic swept the world in 2020 it brought with it added complexities for healthcare workers and facilities. Hospitals saw an increase in hospitalizations, shortages in healthcare personnel, and limited supplies and resources.8 Unfortunately, this impacted healthcare outcomes and more specifically healthcare-associated infections (HAIs). HAI rates that had been trending down began to rise, losing much of the ground gained over the last decade (Table 1). C. diff rates, which were steadily declining in pre-pandemic years, leveled off without significant change. A rise in cases may have been seen if not for infrequent testing for C. diff during the pandemic. Alternatively, practices like enhanced hand hygiene, environmental cleaning & disinfection, patient isolation, PPE use, and a marked decline in outpatient antibiotic prescribing may have helped reduce rates.9 As we move out of the pandemic, there is much to be done if we are to begin reducing these HAI rates once again.
Combating C. diff: Learnings from the C. diff Conference
The annual International C. diff Conference & Health Expo has once again presented opportunities to learn and share relevant work on the topic of C. diff, including insights into this deadly pathogen and ways to combat it. Below, I share just a few learnings from this year’s conference.
- C. diff infections in 2020 were likely underreported due to decreased testing during the pandemic and because diarrhea is also a common symptom of a COVID-19 infection.
- Electrostatic technology used with a sporicide is an effective and efficient environmental disinfection method against C. diff, especially given the current staffing challenges.
- Recent data shows that C. diff infections are on the rise in the community and no longer just seen as a healthcare-associated outcome.
- Antibiotic stewardship works — and not just for C. diff! Lower resistance rates were found in other pathogens after significant reduction in in antibiotic use.
- The critical need for a multifaceted approach of infection prevention and control is needed against C. diff was reemphasized.
Presentations from the conference will be broadcasted each Tuesday from December 7th, 2021 through January 11th, 2022. For more information and to listen in, visit the C. diff. Spores and More Live Broadcast to Podcast program page.
During this month of awareness, let us acknowledge the problem take deliberate infection prevention steps to help us get back on track against C. diff. For more information on combating C. diff, see our C. diff Prevention Toolkit.
References:
1. CDC. Nearly half a million Americans suffer from C. difficile infections in single year. cdc.gov. 2019 [cited 2021 Nov 4]. Available from: https://www.cdc.gov/hai/dpks/deadly-diarrhea/dpk-deadly-diarrhea.html
2. Zimlichman, E.; Henderson, D.; Tamir, O.; Franz, C.; Song, P.; Yamin, C. K.; Keohane, C.; Denham, C. R.; Bates, D. W. JAMA Intern. Med. 2013, 173 (22), 2039–2046.
3. Heinlen L, Ballard JD. Clostridium difficile infection. Am J Med Sci. 2010;340(3):247–52.
4. CDC. What is C. diff? [Internet]. Cdc.gov. 2021 [cited 2021 Nov 4]. Available from: https://www.cdc.gov/cdiff/what-is.html
5. Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Brun-Buisson C. Contamination of healthcare workers’ hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect Control Hosp Epidemiol. 2014;35(1):10–5.
6. Kramer A, Schwebke I, Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis. 2006;6(1):130.
7. CDC. Antibiotic resistance threats in the United States. Cdc.gov. 2019 [cited 2021 Nov 4]. Available from: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
8. Weiner-Lastinger L, et al. The Impact of COVID-19 on HAIs in 2020: Summary of Data Reported to NHSN. ICHE. 2021;1-14.
9. CDC. COVID-19 Impact on HAIs in 2020. cdc.gov. 2021 [cited 2021 Nov 4]. Available from: https://www.cdc.gov/hai/data/portal/covid-impact-hai.html






