After two long years, we finally got to meet together again. Albeit only virtually, it was great to be in the “same room” with the over 3,300 participants from across the globe – many of whom are new to the profession. This blog post will summarize my top two favorite sessions from the 2021 annual APIC conference.
The Joint Commission (TJC) Office Hours
Speaker:
Sylvia Garcia-Houchins, TJC Director of Infection Prevention & Control (IP&C)
In this practical session, a hierarchical approach to infection control (IC) standards (pictured below) was reviewed. The speaker advised participants, when creating or revising IC-related policies, to apply this hierarchy as it will “always get you to the right answer.”
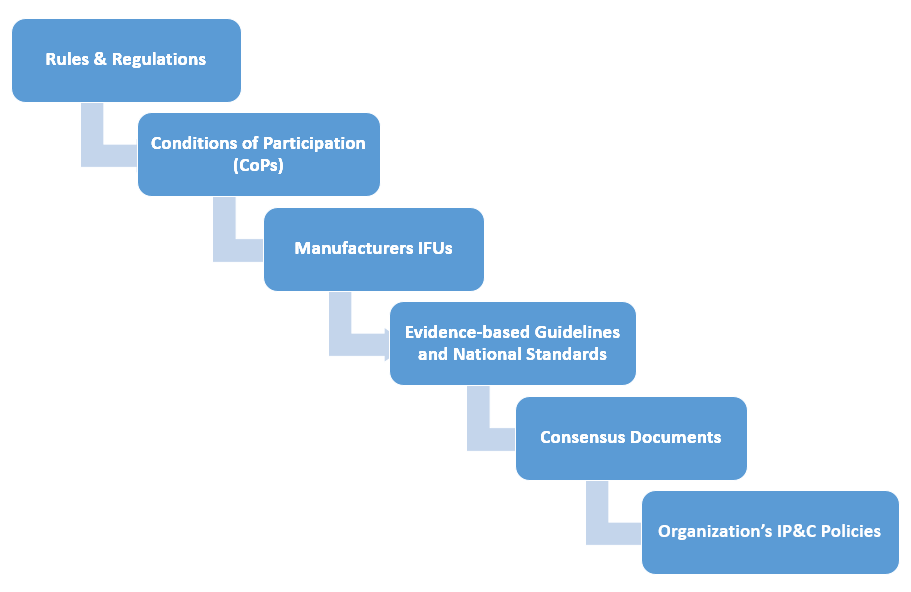
It was interesting to learn that only three evidence-based guidelines are required and they are 1) CDC or WHO Hand Hygiene, 2) CDC Standard Precautions, and 3) CDC Transmission-based Precautions. Beyond these, healthcare facilities may adopt any other evidence-based guidelines (EBG), national standards, or consensus documents of their choosing. Of note, the speaker stated that to be considered an EBG, that the document must have a reference list.
Last, participants were advised to download a copy of the program-specific Centers for Medicare and Medicaid Services (CMS) State Operations Manual which offers day-to-day operating instructions, policies, and procedures based on statutes and regulations, guidelines, models, and directives. Be thoughtful in regards to facility policy content as TJC will hold facilities accountable during surveys to ensure they are doing what they say they will do. For example, if your policy says you follow Association for the Advancement of Medical Instrumentation (AAMI) standards as opposed to CDCs for high level disinfection, you must be compliant with AAMI standards. Of note. AAMI guidelines have no reference list.
Pre-Conference Workshop: IP&C in Long-Term Care (LTC) – The Future is Now
Speakers:
Deb Burdsall, PhD, RN-BC, CIC, FAPIC; Assistant Adjunct Professor, University of Iowa College of Nursing; Manager, Baldwin Hill Solutions LLC, Infection Prevention for Long-Term Care
Teri Hulett, RN, BSN, CIC, FAPIC; Infection Prevention Consultant, Infection Prevention Strategies LLC
Buffy J. Lloyd-Krejci, DrPH, MS, CIC; Owner, IPC Well, LLC; Infection Preventionist
This day-long session was kicked off by calling out the elephant in the room: IP&C in LTC was an issue before the pandemic. In fact, 82% of LTCFs surveyed between 2013 and 2017 were cited for an IP&C deficiency. Infections are the most frequent cause of transfers and readmissions to the hospital. Two very important topics covered in this workshop were 1) Process surveillance and 2) Enhanced Barrier Precautions (EBP). For more information on the latter, see my June HICPAC Hub blog post. Regarding process surveillance, it is the review of staff practices with the purpose to identify whether staff implement and comply with IP&C policies and procedures. It is also required by CMS. Not only do IPs need to perform outcomes surveillance (e.g., healthcare-associated infections), they need to collect data and act on the findings around processes that can lead to infections. A good example is to observe cleaning and disinfection practices and to provide timely feedback to frontline workers.
At the session closing, new IPs who started in the profession during the pandemic were cautioned to be mindful that the IP&C practices observed were not best practices. Reuse of single-use personal protective equipment is a great example. For more on the CMS infection control requirements for LTCFs, see my blog post titled “New CMS Requirements for Long-Term Care Facilities – Are You Ready?”
I will conclude with a reminder inspired by Simon T. Bailey in the closing plenary session: Never forget that you all are diamonds – created under pressure and it is your time to shine!
Let’s grab a cup of coffee next year in Indianapolis, Indiana!


