
Those dreaded words: “The Joint Commission (TJC) is here!” To better align with regulations, to simplify requirements, and to provide for more meaningful survey’s, TJCs Infection Control (IC) chapter for hospital accreditation recently underwent a full rewrite.1 The previous 12 standards with 51 elements of performance (EPs) have been distilled down to just 4 standards with 14 EPs.1 These new standards go into effect on July 1, 2024. One of those standards, IC.07.1.01, is new and will be the focus of this blog with an emphasis on the cleaning and disinfecting requirement.
IC.07.01.01 Preparedness for High-Consequence or Special Pathogens
This standard requires hospitals to implement processes to support preparedness for high-consequence infectious diseases or special pathogens.1 TJC defines these pathogens as:
- novel (“new”) or reemerging infectious agents that are easily transmitted from person-to-person,
- have limited or no medical countermeasures (e.g., vaccine or prophylaxis),
- have high mortality,
- require prompt identification and implementation of infection prevention & control (IPC) activities such as isolation or special personal protective equipment (PPE), and
- require rapid notification to public health authorities and special action2.
Examples of special pathogens include Middle East Respiratory Syndrome (MERS), novel influenzas, and Ebola or other viral hemorrhagic fever diseases.2
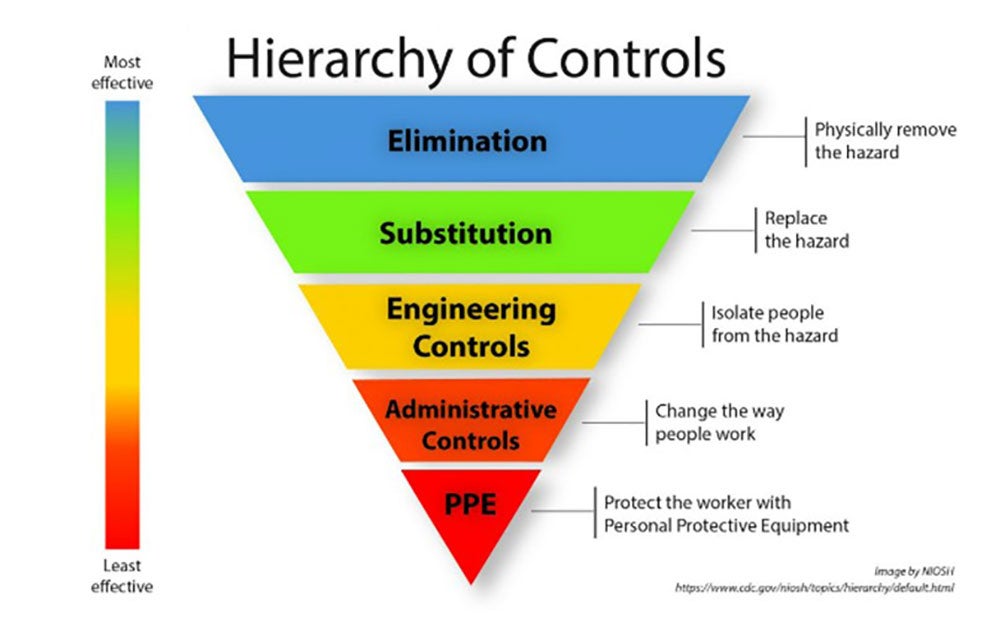
The rationale for this new standard is to ensure a standardized approach to emerging pathogen preparedness that is grounded on the hierarchy of controls and that will strengthen IPC protocols and processes for all infectious threats.3
There are 2 elements of performance (EPs) – which outline the specific actions or processes that must be in place for IC.07.01.011:
- EP 1: The hospital develops and implements protocols for high-consequence infectious diseases or special pathogens. The protocols are readily available at the point of care and address:
- IDENTIFY: Procedures for screening at the points of entry to the hospital for respiratory symptoms, fever, rash, and travel history to identify or initiate evaluation for high-consequence infectious disease or special pathogens.
- ISOLATE:
- Procedures for transmission-based precautions
- Required PPE and donning and doffing techniques
- IPC procedures to support continued and safe provision of care while the patient is in isolation and to reduce exposure among staff, patients, and visitors using the hierarchy of controls
- Procedures for waste management and cleaning and disinfecting patient care spaces, surfaces, and equipment.
- INFORM: Procedures for informing public health authorities and key hospital staff
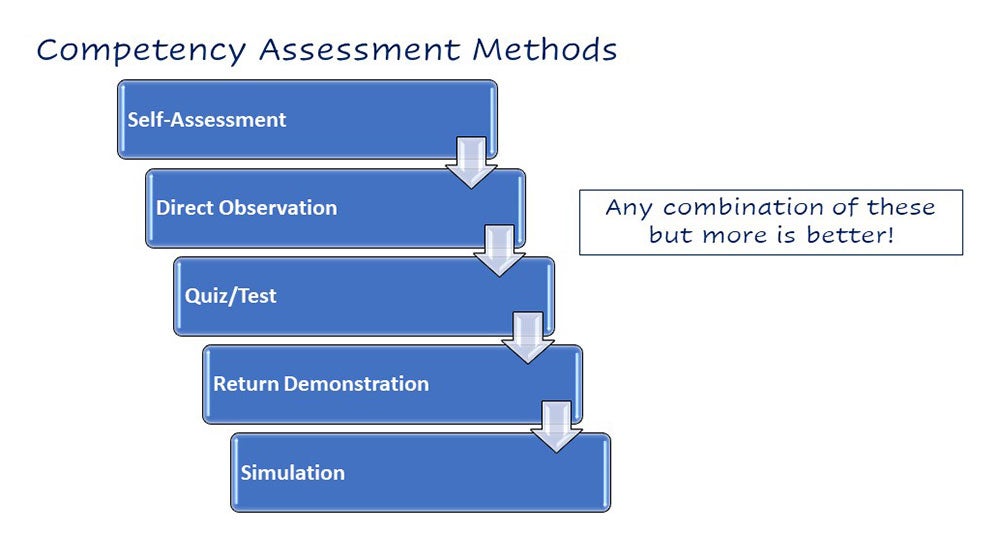
- EP 2: The hospital develops and implements education and training and assesses competencies for the staff who will implement these protocols.
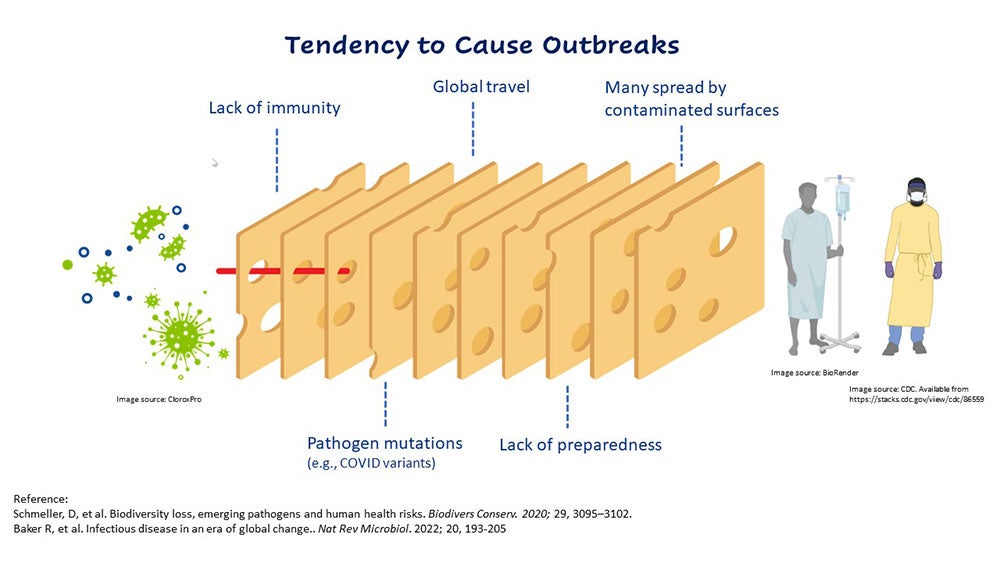
The introduction of IC.07.01.01 is timely — not only because of the COVID-19 pandemic – but because the 21st century world is being impacted by emerging infectious diseases on an unprecedented scale.4 Reasons include climate change, population encroachment on animal living spaces, and increases in global travel and trade.5 In fact, with the speed of today’s global travel, pathogens can be anywhere in the world in a matter of hours.4 In this post-pandemic era, emerging pathogens – including Candida auris and Mpox — continue to be a top concern for IPs, in part because a lack of immunity to novel pathogens often results in high morbidity and mortality.5 And because they are new, there is often no or limited prophylaxis or treatment available.5 For these reasons, emerging pathogens often lead to outbreaks. Preparedness is key to reduce transmission, keep everyone safe, maintain hospital operations, and to strengthen our response as a country.
Hand hygiene and environmental cleaning and disinfection play crucial roles as first lines of defense in preventing pathogen transmission within hospitals. Standardized processes are imperative as they provide consistency. For the best results, it is important that Infection Preventionists (IPs) and Environmental Services professional’s work collaboratively to address some of the nuances around cleaning and disinfecting against emerging pathogens which include:
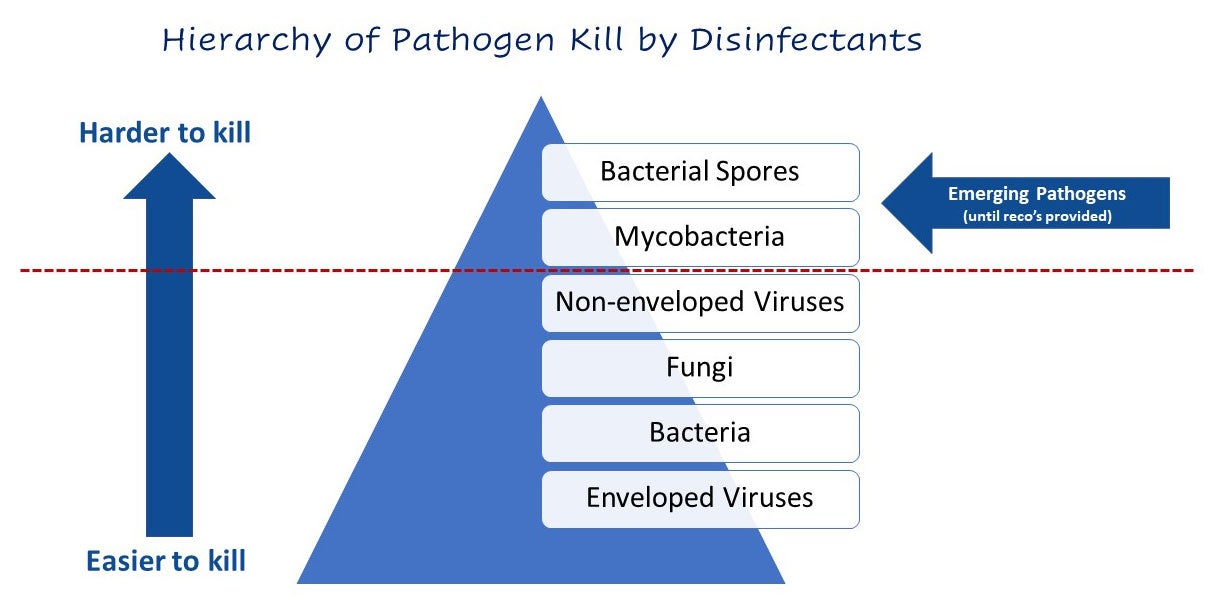
- Product Selection: It is not likely — at least not initially — that there will be a disinfectant on the market with kill claims against a novel pathogen. It takes at least 1 year for new product claims to be approved by the U.S. Environmental Protection Agency (EPA) and added to a products label. To identify appropriate products, IPs should familiarize themselves with the EPA’s Emerging Viral Pathogen Policy and the EPA’s Selected Disinfectant Lists. While awaiting guidance from the Centers for Disease Control & Prevention (CDC), consider the hierarchy of pathogen kill by disinfectants and use an intermediate-level disinfectant such as bleach.
- Protocols: Routine cleaning and disinfection procedures may be insufficient so protocols will need to be developed. Considerations should include6:
- Identification of responsibility for cleaning (e.g., in-house staff vs. contractors)Facility approved EPA-registered healthcare-grade disinfectant(s)PPE requirementsDedicated or disposable cleaning equipment. Note: ready-to-use disposable disinfecting wipes are ideal!Frequency of cleaning and disinfectionLinen and waste management
- Use of adjunct disinfection technology such as ultraviolet light (UV), electrostatic disinfection, or vaporized hydrogen peroxide
- Training, Education, and Competency: There is a need to get staff quickly up to speed on the new pathogen and on any special cleaning requirements (see EP 2 above). Note that there are several ways that competency can be assessed.
Conclusion
TJCs new IC standard, IC.07.01.01, reflects a proactive approach to emerging pathogens. By prioritizing cleaning and disinfection policies, education, training, and competency, hospitals can better protect patients and staff by eliminating the environment as a source of transmission of novel pathogens.
References
The Joint Commission. Prepublication Standards: New and Revised Requirements for the IC Chapter [Internet]. [Cited 2024 Apr 6]. Available from https://www.jointcommission.org/standards/prepublication-standards/new-and-revised-requirements-for-the-infection-prevention-and-control-chapter/
2. The Joint Commission. R3 Report Issue 41: New and Revised Requirements for IPC for Critical Access Hospitals and Hospitals [Internet]. [Cited 2024 Apr 6]. Available from https://www.jointcommission.org/standards/r3-report/r3-report-issue-41-new-and-revised-requirements-for-infection-prevention-and-control-for/
3. The National Emerging Special Pathogens Training and Education Center (NETEC). TJC New Standard for Special and High Consequence Pathogen Preparedness, 2024 Mar 15. Available from https://repository.netecweb.org/items/show/1809
4. Ambat A, Vyas N. Assessment and preparedness against emerging infectious disease among private hospitals in a district of South India. Open Access: Med J Armed Forces India. 2022;78(1):42-46.
5. Schmeller, D, et al. Biodiversity loss, emerging pathogens and human health risks. Biodivers Conserv. 2020; 29, 3095–3102.
6. The National Emerging Special Pathogens Training and Education Center (NETEC). Considerations for Terminal Cleaning and Decontamination of Suspected or Confirmed Special Pathogen Care Rooms [Internet]. [Cited 2024 Apr 6]. Available from https://repository.netecweb.org/exhibits/show/jointcommission/item/1772






