About a year ago, we posted a blog on long-lasting or residual antimicrobial product claims. Since then, there have been some significant developments. At the time, the Environmental Protection Agency (EPA) did not have a method to approve long-lasting virus claims for these types of products. In the midst of the pandemic and with confusion about disinfection rampant, many companies improperly advertised products that supposedly provided residual kill against SARS-CoV-2 on surfaces. As the pandemic continued, the EPA recognized the importance of residual efficacy claims in general and for viruses in particular, and they have since made two important updates: (1) the EPA now allows residual virus claims on product labels, and (2) the EPA released guidance on how to add a new type of residual claim to product labels, called “supplemental residual antimicrobial” claims (more on this below). This article will help you sort through the new guidance on residual or long-lasting claims.

What types of EPA-registered residual efficacy claims can a product have and what do they mean?
Here’s how we interpret the EPA’s updated guidance on adding residual claims to product labels.1 There are three types of residual, or long-lasting, claims that you may encounter on product labels (Table 1). These include residual self-sanitization, residual self-disinfection, and supplemental residual antimicrobial activity. Each of these product claims requires data submission to the EPA and approval before they can be listed on a product’s label. These products are also tested for durability to make sure that they aren’t removed during normal cleaning procedures.
Products with residual self-sanitization or self-disinfection claims also have regular disinfection claims, meaning that they kill bacteria and/or viruses on contact. Residual self-sanitization and residual self-disinfection claims are very similar. The key difference is that residual self-sanitization claims are only valid for bacteria, while residual self-disinfection claims can be obtained for both bacteria and viruses. To meet the criteria for a residual self-sanitization claim, products must demonstrate 99.9% kill of bacteria on surfaces within a 10-minute contact time, and last for up to 24 hours following application. To meet the criteria for a residual self-disinfection claim, products must demonstrate 99.999% kill on surfaces for bacteria or 99.9% kill for viruses, within a 10-minute contact time, and last for up to 24 hours on surfaces.
Products with a supplemental residual antimicrobial claim may not kill microorganisms when first applied to surfaces but do provide microorganism kill within a two hour contact time, and continue to provide kill for up to weeks or months. However, because the level of kill is significantly lower than that of a disinfectant, these products can only be used as a supplement to EPA-registered disinfectants. According to the EPA, this means that you will still need to use an EPA-registered disinfectant for regular surface disinfection.
Table 1. EPA-registered residual product claims
| Claim | Description | What to Look for on Label | Product Example |
| Residual self-sanitization | Product kills 99.9% of bacteria on surfaces for up to 24 hours following application. Must demonstrate residual kill within a 10-minute contact time. | “residual sanitization” or “residual sanitizer” | Spray product that disinfects when applied and continues to kill 99.9% of bacteria up to 24 hours after application. |
| Residual self-disinfection | Bacteria: product kills 99.999% of bacteria on surfaces for up to 24 hours following application. Viruses: product kills 99.9% of viruses on surfaces for up to 24 hours following application. Must demonstrate residual kill within a 10-minute contact time. | “residual disinfection” or “continuous disinfection” | Spray product that disinfects when applied and continues to kill 99.999% bacteria for up to 24 hours after application. |
| Supplemental residual antimicrobial | Products with this claim are eligible to be used as a supplement to routine application of EPA-registered disinfectants. These products are not disinfectants and cannot be used as a replacement for regular disinfection. Continues to kill 99.9% of bacteria and/or viruses for up to weeks or months. Must demonstrate residual kill within a 2-hour contact time. | “Kills 99.9% of Staphylococcus aureus within 2 hours of exposure when used as part of a comprehensive infection control program/protocol” | Copper-impregnated surfaces, paints |
How do I determine whether a product has EPA-registered residual claims?
Here is how to find and search a product’s master label to determine which residual claims a specific product carries:
- Navigate to the EPA’s Pesticide Product Labeling System (PPLS) website.2
- Enter the product’s EPA registration number into the field labeled “EPA Registration, Distributor Product, or Special Local Need Number:” and click “Search.” Companies should be able to provide this number to you, or it may appear on their product website. An example of an EPA registration number is “67619-38.”
- Open the most recent master label. The EPA includes the full history of master labels for each product, but only the most recent one will have all of the currently approved claims.
- Search the label for the key terms listed in Table 1. Terms like “residual disinfection,” “continuous disinfection,” “residual sanitization,” or “residual self-sanitizer” must appear on labels that have approved residual self-sanitization or residual self-disinfection claims. Read the terms of the claim, including how often the product must be reapplied.
Which residual antimicrobial products can I use against SARS-CoV-2?
For a list of residual products that can be used against SARS-CoV-2, the EPA recommends searching EPA List N: Disinfectants for Use Against SARS-CoV-2 (COVID-19)3 for products with the formulation type “residual”. Note that supplemental residual antimicrobial products will not appear on List N, although they may appear in the EPA’s supplement to List N.4 And finally, note that if you see products that have “static” claims like “bacteriostatic,” “mildewstatic,” or “fungistatic,” these are not the same as residual disinfection claims. A “static” claim is for non-public health uses and means that the product inhibits the growth of bacteria or fungi on surfaces, but doesn’t kill those organisms for a certain length of time after application.
For more information on the new residual product guidance, see the EPA website.1
References
1. Interim Guidance - Review for Products Adding Residual Efficacy Claims | Pesticide Registration | US EPA https://www.epa.gov/pesticide-egistration/interim-guidance-review-products-adding-residual-efficacy-claims (accessed 2021 -06 -09).
2. Pesticide Product and Label System | US EPA https://oaspub.epa.gov/apex/pesticides/f?p=PPLS:1 (accessed 2021 -06 -09).
3. List N Tool: COVID-19 Disinfectants | US EPA https://cfpub.epa.gov/wizards/disinfectants/ (accessed 2021 -06 -09).
4. List N Appendix: Supplemental Residual Antimicrobial Products for Coronavirus (COVID-19) | Pesticide Registration | US EPA https://www.epa.gov/pesticide-registration/list-n-appendix-supplemental-residual-antimicrobial-products-coronavirus (accessed 2021 -06 -09).
With the ongoing pandemic and the flu season around the corner, it’s important to develop a plan for using disinfectants efficiently and effectively. There’s a time and place for cleaning, and a time and place for disinfection, and doing the right amount of each can help safeguard public health. During the pandemic, disinfectant use is on the rise, and there is a growing conversation around overuse of disinfectants.

To address this concern and make the most of the limited products available during the pandemic, it’s important to target disinfection to the surfaces and places where it is needed most. Depending on the type of facility and how people are using that facility, some areas might require cleaning only, while others may need both cleaning and disinfection. Smart disinfection—that is, targeting disinfectants to when and where they are needed most—can help conserve disinfectants and maximize protection for the people who use those spaces.
Cleaning, Sanitizing and Disinfecting
Before deciding on a plan for smart disinfection, it’s important to know the difference between cleaning, sanitizing, and disinfecting. Cleaning is the physical removal of dirt and debris from surfaces. Cleaning products contain a surfactant or detergent to break up dirt and debris, but are not Environmental Protection Agency (EPA) registered. Cleaning products cannot make claims to kill bacteria or viruses on surfaces. Sanitizers and disinfectants contain an antimicrobial active ingredient and are EPA registered. Sanitizers reduce the number of bacteria on surfaces, but cannot make claims against viruses, so they cannot be used to kill for example SARS-CoV-2, the virus that causes COVID-19. Disinfectants can be registered to kill bacteria, fungi and viruses on surfaces, including SARS-CoV-2. Some products are one-step cleaner disinfectants, meaning that they contain both surfactants and an antimicrobial ingredient, so they can clean and disinfect in the same step.
When and Where to Disinfect
Manual disinfectants like wipes and trigger sprays are great tools for regular disinfection of spaces and surfaces that people touch frequently throughout the day. In schools for example, it makes sense to disinfect desks, doorknobs and other high-touch surfaces by wiping or spraying them in between classes, but you may not need to disinfect every surface in every room throughout the day. On the other hand, high traffic areas like restrooms may need to be disinfected top to bottom, multiple times throughout the day. According to the Centers for Disease Control and Prevention (CDC), high-touch surfaces that may require frequent disinfection throughout the day include tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.1,2
Thorough cleaning and disinfection of the entire facility usually happens after hours, after building occupants have gone home. This process could involve cleaning (such as vacuuming and dusting), followed by manual disinfection with wipes, trigger sprays or dilutable disinfectants.
For extra assurance that all surfaces are disinfected, electrostatic spray disinfection can be added to and even replace parts of this routine. For example, you could clean high-touch surfaces in classrooms, and then use an electrostatic sprayer to apply a disinfectant quickly and evenly to all surfaces in the room. This could include soft surfaces or surfaces that are difficult to thoroughly clean, such as chairs and desks. Electrostatic spraying can also be used as a substitute for manual wipes and sprays in areas that are large and hard to disinfect manually, such as restrooms, locker rooms or cafeterias. Keep in mind however that high-touch surfaces should still be the focus when using an electrostatic sprayer in public spaces. For example, although walls and floors can be disinfected, these areas may only require cleaning depending on the facility type and room traffic.
Develop a Smart Disinfection Plan
To develop a smart disinfection plan, first determine which surfaces and areas in your facility need to be disinfected. Once you’ve identified the areas and surfaces in your facility that need to be disinfected, you can develop a plan to decide when those surfaces should be disinfected and by whom. Let staff know who is responsible for each area, and what needs to be done in that area. Checklists are a great tool to help staff and managers keep track of what has been done throughout the day. Staff should also be trained on the safe use of disinfectants. Disinfectants are safe when used as directed, so it’s important to always follow label instructions for use. Appropriate personal protective equipment should also be worn by the operators applying disinfectants.
If you need guidance to help you complete your smart disinfection plan, there are several comprehensive tools and resources available. For example, the CDC has guidance on cleaning and disinfecting public spaces, offices and businesses, schools, and homes that includes a disinfection decision tree.3 For educational facilities, there are multiple resources available on cleaning and disinfection, including information on how to open facilities safely.4,5
For the latest information on COVID-19 and variants, visit our CloroxPro COVID-19 Hub.
References
1. Centers for Disease Control and Prevention (CDC). Cleaning and Disinfecting Your Facility https://www.cdc.gov/coronavirus/2019-ncov/community/disinfecting-building-facility.html (accessed Sep 3, 2020).
2. Centers for Disease Control and Prevention (CDC). Cleaning And Disinfecting Your Facility https://www.cdc.gov/coronavirus/2019-ncov/community/disinfecting-building-facility-H.pdf (accessed Aug 28, 2020).
3. Centers for Disease Control and Prevention (CDC). Guidance for Cleaning and Disinfecting https://www.cdc.gov/coronavirus/2019-ncov/community/cleaning-disinfecting-decision-tool.html (accessed Aug 28, 2020).
4. National Education Association; The Clorox Company. Cleaning , Sanitizing , and Targeted Disinfecting in the Classroom.
5. Centers for Disease Control and Prevention. Guidance for Cleaning and Disinfecting https://www.cdc.gov/coronavirus/2019-ncov/community/pdf/Reopening_America_Guidance.pdf.
As the COVID-19 pandemic continues, some companies are advertising cleaning services using antimicrobial products that they claim will continue to kill SARS-CoV-2 (the virus that causes COVID-19) on surfaces for days, weeks, or even months. Before you consider using these products or services, it’s important to understand what these claims really mean, what types of pathogens they relate to, and what claims the Environmental Protection Agency (EPA) does and does not allow. This article will help sort through the myths and facts around what are called residual or long-lasting claims.

What types of EPA-approved residual efficacy claims can a product have and what do they mean?
There are three types of residual, or long-lasting claims, that can appear on a product’s EPA approved master label (Table 1).
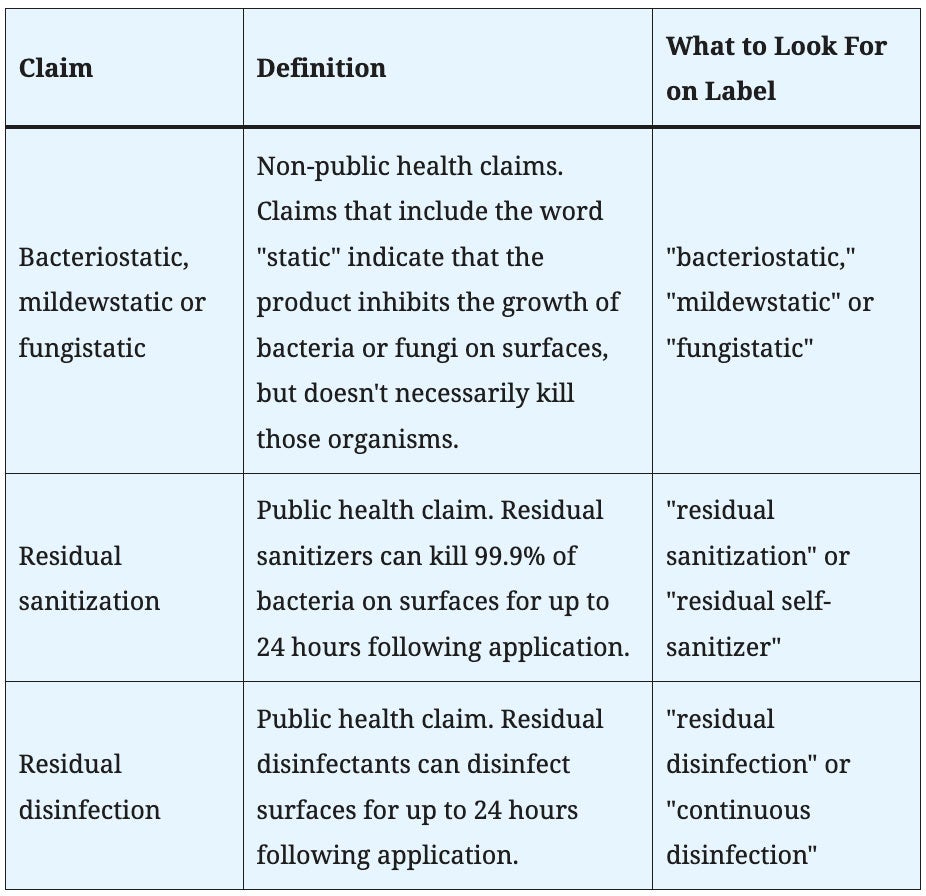
Note that all of these claims apply only to bacteria or fungi, and not to viruses. Therefore, these claims are not sufficient to support use against viruses, including SARS-CoV-2. Residual sanitization and residual disinfection claims are considered public health claims meaning they imply a direct impact on human health. These claims require data submission and approval before they can be listed on the product’s EPA master label. “Static” claims like “bacteriostatic,” “mildewstatic” and “fungistatic” are non-public health claims, meaning they do not imply a direct impact on human health. These claims do not require data submission to the EPA for approval at the federal level. However, some states may require data approval in order to make claims in that state.
What are “treated articles”?
In addition to antimicrobial products with residual claims, you may also encounter products with resistant or protection claims, known as treated articles. These treatments can be incorporated into surfaces (e.g., an odor resistant trash bag) or applied to surfaces (e.g., a protective surface coating) to protect the surface itself. The claims for treated articles are commonly used to address aesthetics such as discoloration, stains, or odors. Products that are found to have treated article claims will not have an EPA registration. According to the EPA, “treated articles cannot claim they are effective against viruses and bacteria that cause human illness. This means they are not appropriate for controlling COVID-19.”1
How do I determine whether a product has EPA-approved residual efficacy claims?
To determine which residual efficacy claims a specific product carries, look up the EPA master label and search it for the key terms listed in Table 1. Products that do not make public health claims may not be EPA registered, and should not be used to kill microorganisms on surfaces. If the product is registered, here is how to find and search a product’s master label: 2
- Navigate to the EPA’s Pesticide Product Labeling System (PPLS) website.
- Enter the product’s EPA registration number into the field labeled “EPA Registration, Distributor Product, or Special Local Need Number:” and click “Search.” Companies should be able to provide this number to you, or it may appear on their product website. An example of an EPA registration number is “67619-38.”
- Open the most recent master label. The EPA includes the full history of master labels for each product, but only the most recent one will have all of the currently approved claims.
- Search the label for key terms. Terms like “residual disinfection,” “continuous disinfection,” “residual sanitization” or “residual self-sanitizer” must appear on labels that have approved residual sanitization or residual disinfection claims. Read the terms of the claim, including how often the product must be reapplied.
What is the EPA doing about residual claims in light of the pandemic?
The EPA recognizes the importance of residual kill claims against viruses in light of the COVID-19 pandemic, so they are investigating the possibility of adding these types of claims to certain product labels.3 However, until the EPA provides a clear path to obtaining residual efficacy claims against viruses, companies should not be advertising these types of claims.
Which products can I use against SARS-CoV-2?
For a full list of products that can be used against SARS-CoV-2, see EPA List N: Disinfectants for Use Against SARS-CoV-2 (COVID-19).4 List N includes products that have demonstrated efficacy against:
- SARS-CoV-2
- at least one virus that is harder to kill than SARS-CoV-2 (Emerging Viral Pathogens Claim)
- a human coronavirus similar to SARS-CoV-2
- a harder to kill pathogen (specifically norovirus, Mycobacterium bovis/Mycobacterium tuberculosis)
All of these products are approved for disinfection of hard non-porous surfaces, but they should not be used for residual disinfection of viruses, including SARS-CoV-2.
To learn about EPA’s List N in an ever-changing environment, please read this blog post by Associate Research Fellow, Richard Lowe.
For the latest information on COVID-19 and variants, visit our CloroxPro COVID-19 Hub.
References
1. U.S. Environmental Protection Agency. Is there anything I can do to make surfaces resistant to SARS-CoV-2? https://www.epa.gov/coronavirus/there-anything-i-can-do-make-surfaces-resistant-sars-cov-2 (accessed Jul 20, 2020).
2. U.S. Environmental Protection Agency. Pesticide Product and Label System https://oaspub.epa.gov/apex/pesticides/f?p=PPLS:1 (accessed Jul 20, 2020).
3. U.S. Environmental Protection Agency. Longer-Term SARS-CoV-2 Disinfection Evaluation https://www.epa.gov/healthresearch/longer-term-sars-cov-2-disinfection-evaluation (accessed Jul 20, 2020).
4. U.S. Environmental Protection Agency. List N: Disinfectants for Use Against SARS-CoV-2 (COVID-19) https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2-covid-19 (accessed Jul 24, 2020).
Candida auris (C. auris) is receiving national media attention, and was a hot topic at the recent SHEA 2019 and APIC 2019 conferences, where infection prevention researchers discussed how to control and prevent potentially deadly and costly infections caused by this healthcare-acquired fungus.

C. auris is top of mind for healthcare facilities because of continued outbreaks and difficulty in controlling and preventing C. auris infections. This threat is particularly concerning because of the emergence of multidrug and panresistant strains, difficulty in properly diagnosing infections, long colonization time, and because it can be difficult to kill with surface disinfectants.
C. auris was first recognized as an emerging threat in 2009, and infections have been reported in more than 20 countries since that time. In the U.S., infections have appeared primarily in New York, New Jersey, and Illinois. But, previous pathogen outbreaks have spread quickly across the U.S., and it is likely that C. auris will follow suit.
From a surface disinfection standpoint, C. auris has been shown to persist on environmental surfaces for at least seven days (some sources have suggested up to 30 days), and shared and mobile equipment have been implicated in the spread of this pathogen in healthcare facilities.
There are currently very few disinfectants that carry claims against C. auris on label. Because of this, the Centers for Disease Control and Prevention (CDC) currently recommends using a disinfectant with a claim against Clostridioides difficile (C. diff) spores. Most of these disinfectants can be found on the Environmental Protection Agency’s (EPA) List K, which is a list of registered hospital-grade disinfectants effective against C. diff spores.
List K currently includes mostly bleach-based products; however, the CDC notes that some alternate disinfectants with other active ingredients like hydrogen peroxide have been shown to kill C. auris, as demonstrated in a recent article published by Dr. Curtis Donskey at Louis Stokes Cleveland VAMC.
The CDC also cautions that quaternary ammonium-based disinfectants may not be effective against C. auris, which Dr. Donskey’s study confirms. Additionally, they note that limited data is available on the effectiveness of UV. However, some UV devices have been shown to be effective against C. diff, and may be an effective adjunct for C. auris disinfection.
For more on C. auris, see the CDC website. The EPA’s List K can be found on the EPA website. To read the full studies discussed in this article, see Cadnum, et al., 2018, Piedrahita, et al., 2017, and Rutala, et al., 2017.