The importance of environmental hygiene has never been greater than it is today. With our focus on a single pathogen over the past two years, other pathogens have gotten away from us. The U.S. lost a decade of progress in the reduction of healthcare-associated infections (HAI), including Clostridioides difficile and multidrug-resistant organisms (MDROs).1 Candida auris, an emerging threat, saw an 85% increase in clinical cases in 2020 from the previous year.2 This particular pathogen has a very high mortality rate, persists in the environment, and has proven to spread rapidly in and between healthcare facilities. With nearly 80% of all infectious diseases being spread by contact (or touch), addressing environmental transmission of pathogens is as important as any other patient safety activities, including the implementation of bundles and stewardship programs.3 This article will introduce a new framework, highlighting the importance of environmental hygiene and elevating it to that of well-established bundles and stewardship programs.
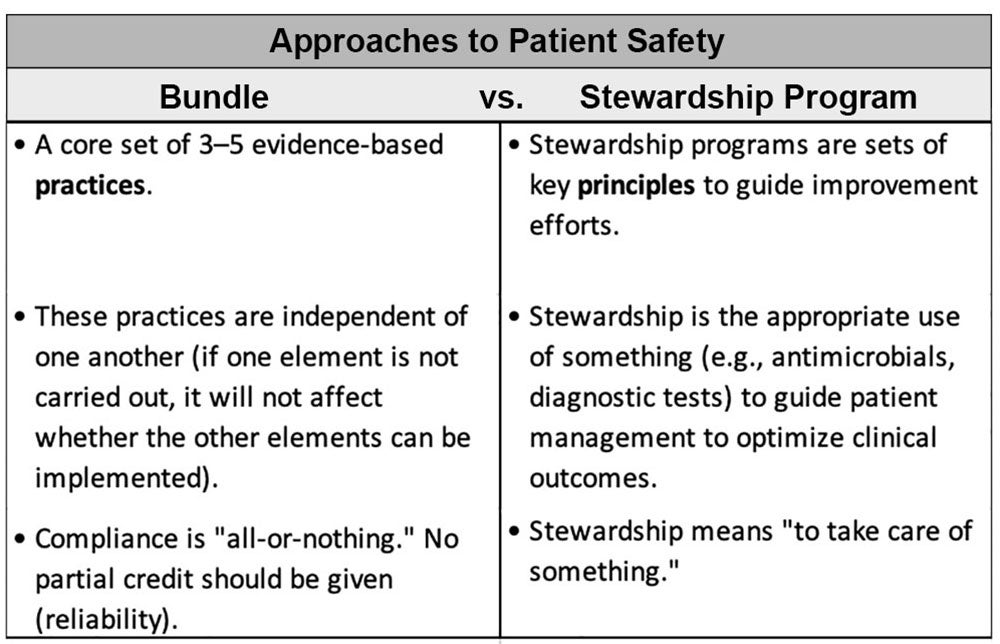
So, what is a bundle? The concept of bundles was developed in 2001 by the Institute for Healthcare Improvement (IHI) as an improvement tool. The earliest bundles targeted prevention of central line-associated bloodstream infection (CLABSI) and ventilator-associated pneumonia (VAP). A bundle is a core set of accepted evidence-based practices that when implemented together result in significantly better outcomes (e.g., HAI rates), than when implemented alone. Bundles are just one strategy among many towards preventing patient harm.4
Other strategies for patient safety are stewardship programs. Stewardship means “to take care of something.” A stewardship program is a set of key principles to guide improvement efforts. Two of the most common stewardship programs are antimicrobial stewardship and diagnostic stewardship — both are intended as a means to combat antimicrobial resistance. For example, antimicrobial stewardship programs aim to preserve antimicrobials for future use by preventing over- and inappropriate use. We saw during the pandemic resources being redirected from stewardship to COVID-19 related activities. But with increases in HAIs and MDROs during this time, we must again prioritize our stewardship efforts.
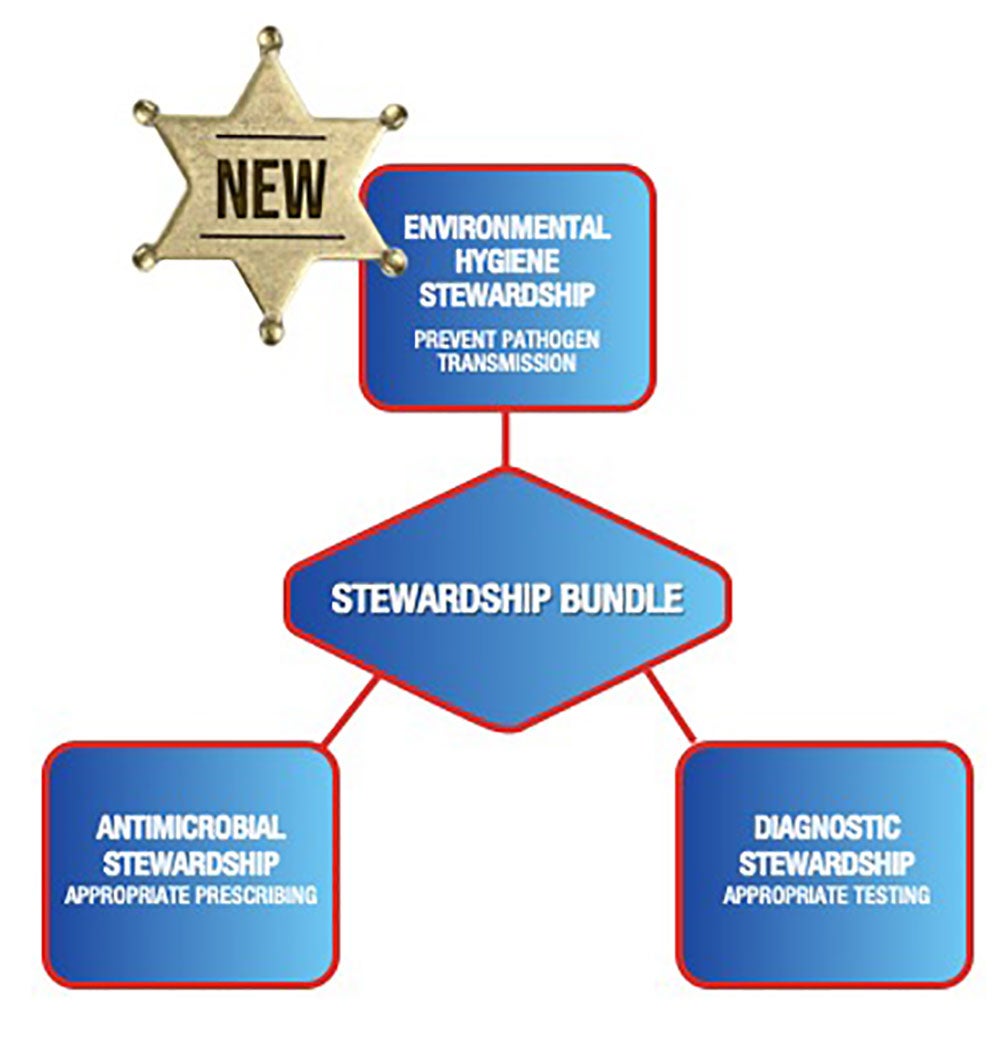
This brings us to the new framework which I call the “Stewardship Triad” (see figure). Part of this 3-pronged bundle of stewardship programs is a new stewardship program: Environmental Hygiene Stewardship. The key evidence-based practices for this program include:
- Provision of a clean and sanitary facility,
- Purchasing cleanable equipment and furnishings,
- Selection of the right products,
- Use of evidence-based cleaning policies and protocols,
- Provision of education, training, and competency assessment,
- Adherence to disinfectant instructions for use (IFUs) and also equipment care guides for cleaning and disinfection,
- Cleaning performance and quality monitoring, and
- Use of no-touch disinfection technologies.
Stewardship Triad to Reduce Environmentally Spread Pathogens (including MDROs & C. difficile)
A stewardship bundle for the post-antibiotic era
*NEW* Environmental Hygiene Stewardship Core Elements
- Provision of clean and sanitary facility
- Purchasing cleanable equipment and furnishings
- Selection of the right products
- Use of evidence-based cleaning policies and protocols
- Provision of education, training and competency assessment
- Adherence to disinfectant IFUs and also equipment care guides for cleaning
- Monitoring cleaning performance and quality
- Use of no-touch disinfection technology
Antimicrobial Stewardship Core Elements
- Dedicate program resources
- Appoint program leaders with clear goals and objectives
- Engage key staff members
- Have expertise in pharmacy practices
- Identify interventions, then implement, audit and solicit feedback
- Educate prescribers, pharmacists, nurses
- Monitor prescribing practices and outcomes
- Reports antibiotic usage and resistance on a regular basis to inform stakeholders
Diagnostic Stewardship Core Elements
- Draft SOPs to guide good lab practices
- Order appropriate tests at the right time
- Collect, store, transport and reject specimens in timely manner
- Report test results in an accurate and timely manner
- Identify pathogen to inform correct and timely treatment
- Develop and implement antibiograms
- Train and educate MDs, pharmacists, nurses on best practices
High compliance with environmental hygiene stewardship means breaking the chain of infection and by doing so, lessening the need for antimicrobial and diagnostic stewardship. Environmental hygiene stewardship not only elevates the importance of cleaning and disinfection but also our hard-working environmental services professionals.
References
1. Weiner-Lastinger LM, Pattabiraman V, Konnor RY, Patel PR, Wong E, Xu SY, et al. The impact of COVID-19 on healthcare-associated infections in 2020: A summary of data reported to NHSN. Infection Control & Healthcare Epidemiology. 2020; 1-14.
2. Centers for Disease Control and Prevention. Tracking Candida auris. [Internet]. [cited 2020 Feb 15]. Available from https://www.cdc.gov/fungal/candida-auris/tracking-c-auris.html.
3. Tierno, P. The Secret Life of Germs. New York, NY, USA: Atria Books, 2001.
4. Resar R, Griffen FA, Haraden C, Nolan TW. Using Care Bundles to Improve Health Care Quality, 2012 [Internet]. [cited 2022 Feb 15]. Available from http://www.ihi.org/resources/Pages/IHIWhitePapers/UsingCareBundles.aspx.






