This is the first post of a three-part blog series, COVID-19: Transition from Hospital to Home, by Doe Kley. Read part two and part three.
Transitioning from hospital to home once diagnosed with an infectious disease can be frightening for a patient. The biggest concern is spreading the infection to their loved ones. This blog post focuses on SARS-CoV-2, the virus responsible for COVID-19. In addition to providing some information on this pathogen and the infection that it causes, key things to consider when it’s time to go home for preventing transmission to others will be addressed.
About COVID-19
According to the National Institute for Allergy and Infectious Diseases (NIH), over the past 20 years, three new pathogenic Coronaviruses have emerged from animal reservoirs.1 They are a large family of viruses that commonly cause respiratory illnesses in people as well as in many different animal species.2 Examples include Severe Acute Respiratory Distress Syndrome (SARS) back in 2003 and more recently, Middle Eastern Respiratory Syndrome (MERS).2 The COVID-19 strain, genetically related to the SARS virus, has not been identified in humans until now.3 Our lack of immunity to this virus explains its readiness to spread from person-to-person.
And how is this virus spread? Well, the primary mode is through respiratory droplets when an infected person coughs or sneezes.4 These droplets have about a 6 foot reach.4 While there is some evidence that persons without any symptoms can transmit the virus, persons are most infectious when they are actively ill.4 Additionally, it appears to be possible to acquire COVID-19 by touching surfaces or objects contaminated with the virus and then touching your mouth, nose, or eyes5, but this is not thought to be the main way that this virus is spread.4 Studies are being published at lightning speed and indicate that the virus can survive from several hours to several days on various surfaces.6 Finally, it’s important to point out that this virus is not spread through food or water.
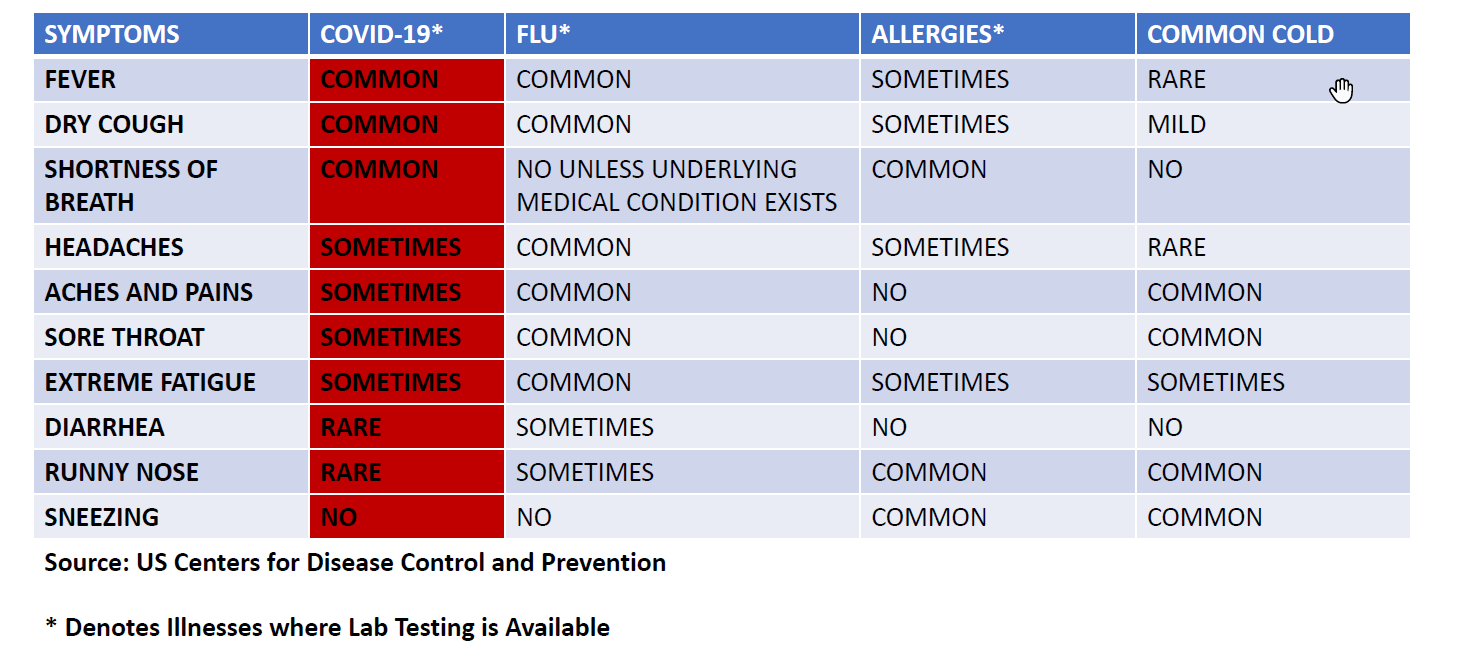
Symptoms of COVID-19 illness are very similar to influenza and include fever, cough, muscle aches, fatigue, and shortness of breath.6 However, the incubation period is longer than influenza ranging from 2-14 days (average of 4-5 days).6,7 Influenza and COVID-19 illnesses both come on more suddenly as compared to the common cold which tends to come on more gradually. Like influenza, COVID-19 illness can range from mild to severe.8
Coronavirus Symptom Comparison with Other Respiratory Illnesses
The vast majority of persons (80%) with COVID-19 infection will experience only mild illness and will recover uneventfully.9 Persons at high-risk of complications from this disease tend to have more severe illness.10 These high-risk individuals include those over the age of 60 years and those with chronic conditions such as heart or lung disease and diabetes.10 Of the older population, those over the age 80 years are at highest risk of complications from COVID-19.10 Currently, there is no specific treatment to cure COVID-19 and there is no vaccine but experts are currently working on both. The mortality rate in the US is approximately 1.3%.10 This means we can expect approximately 1.3 persons in every 100 cases to die as a result of the infection. While this does not seem like a high mortality rate, keep in mind that this is an average. The mortality rate is significantly higher in high risk individuals and lower in low risk individuals.
The Chain of Infection
A framework that can help us to understand how infections occur is the “chain of infection” which describes the sequence of events that must occur in order for an infection to occur. This chain applies to all pathogens. When considering this framework, envision the links of a chain connected in a continuous circle in which the cycle repeats itself unless or until broken.
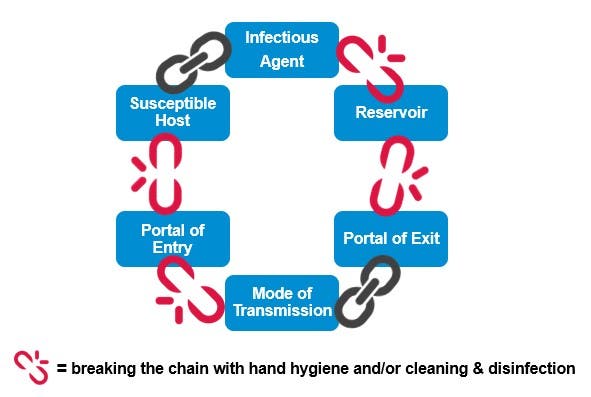
The chain of infection is made up of six links. Each link must align in order for an infection to occur, starting with an infectious agent such as SARS-CoV-2, the virus responsible for COVID-19. The second link is the reservoir for the infectious agent. Reservoirs can include people, environmental surfaces, water, air, and so on. And there must be a portal of exit (which is the third link) for the pathogen from its reservoir. An example of a portal of exit would be the respiratory tract of a coughing patient infected with COVID-19. The fourth link is the mode of transmission. This is how the infectious agent or pathogen is carried from one place or person to another. For example, COVID-19 is spread in the droplets of saliva or mucous coughed out from an infected person. And if those droplets land on and contaminate an environmental surface, the virus can potentially be transmitted by touching that surface and then rubbing one’s eyes or nose. The fifth link in the chain is the portal of entry. This is how the pathogen enters its host or a susceptible person. The portal of entry for the COVID-19 virus is when a susceptible person breathes in the virus carried in droplets from an infected person coughs, sneezes, sings, or talks. The final link is a susceptible host. This is a person who is not immune to or is otherwise susceptible to the infectious agent they are exposed to. In essence, since COVID-19 is caused by a new strain of Coronavirus, we all are susceptible hosts to some degree.
The good news is that we can stop infections from occurring by breaking just one link in the chain. This can easily be accomplished through actions such as covering coughs, performing frequent hand hygiene, cleaning and disinfecting environmental surfaces routinely, and keeping current on immunizations. For COVID-19, we can break the chain of infection for (and possibly put the brakes on this pandemic) by doing these things plus practicing social distancing – keep at least six feet from others and wear a mask. Remember, my mask captures my droplets which protects you and your mask captures your droplets which protects me.
Read part two of this blog series where we discuss preventing the spread of COVID-19 in the hospital, as well as at home.
For the latest information on COVID-19 and variants, visit our CloroxPro COVID-19 Hub.
References
- Coronaviruses. Retrieved from https://www.niaid.nih.gov/diseases-conditions/coronaviruses
- Coronavirus Disease 2019: Frequently Asked Questions. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/faq.html
- Disease 2019: How it Spreads. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/prepare/transmission.html.
- New coronavirus stable for hours on surfaces. Retrieved from https://www.nih.gov/news-events/news-releases/new-coronavirus-stable-hours-surfaces.
- COVID-19, FAQ, Spread. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/faq.html#:~:text=At%20this%20time%2C%20CDC%20has,Coronavirus%20Spreads%20for%20more%20information.
- Coronavirus Disease 2019: Symptoms. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html
- Are You at Higher Risk for Severe Illness? Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/specific-groups/high-risk-complications.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhigh-risk%2Fhigh-risk-complications.html
- Severe Outcomes Among Patients with COVID-19 – United States, February 12-March 16, 2020. Retrieved from https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm
- COVID-19 Cases in U.S. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- CDC Media Telebriefing: Update on COVID-19, March 9, 2020. Retrieved from https://www.cdc.gov/media/index.htmlhttps://emergency.cdc.gov/coca/calls/2020/callinfo_013120.asp






