Healthcare Habits: Refocusing on the Basics of Environmental Cleaning and Disinfection

Healthcare facilities are required to provide a sanitary and safe environment for patients1
The challenges from the pandemic caused priorities to shift temporarily, but it is critical to return attention to cleaning and disinfection practices as part of an active infection prevention program. When performed properly, cleaning and disinfection allows for better patient outcomes by limiting the spread of harmful pathogens from contaminated surfaces and disrupting the chain of infection thus reducing the risk of healthcare-associated infections (HAIs).
Staffing shortages, lack of procedures, and supply issues have put patients at risk
Recent studies have shown that nearly 20% of outpatient facilities lacked procedures to properly perform cleaning and disinfection2. It was also found that deficiencies in healthcare facilities related to standardization of practices and inadequate training led to compliance issues3. Other more recent challenges such as supply and staffing shortages only further complicate an already complex process. It is shortcomings such as these that can lead to process gaps, inefficiencies, and ultimately risk to patients.
Basic strategies for compliance: educate, plan, evaluate, improve
Below are strategies to reinforce the basics of cleaning and disinfection while engaging staff and promoting increased compliance.
-
Education & Training
Comprehensive training provides the opportunity for staff to be engaged in the education process, both observing and performing necessary cleaning and disinfecting steps. A vital part of this also includes learning about various cleaning and disinfecting products and their use and application. A demonstration of proficiency should also accompany completed training. -
Procedures
To have a successful program, ensure clear expectations are set. This may include having readily available written policies, procedures, and protocols. All processes must be realistic and achievable while maintaining consistent practices for continuity. Safety should be top of mind and an understanding of potential health hazards, required personal protective equipment (PPE), and instructions for use (IFU) is necessary prior to cleaning and disinfection. -
Planning
Before cleaning and disinfection are to begin, assess the situation and determine the need and requirement. Decide which cleaner or disinfecting product is appropriate for the setting and/or pathogens (i.e., sporicidal in a C. difficile room) to be rendered safe. Always consider product availability, ease of use, and compatibility before proceeding. -
Evaluation
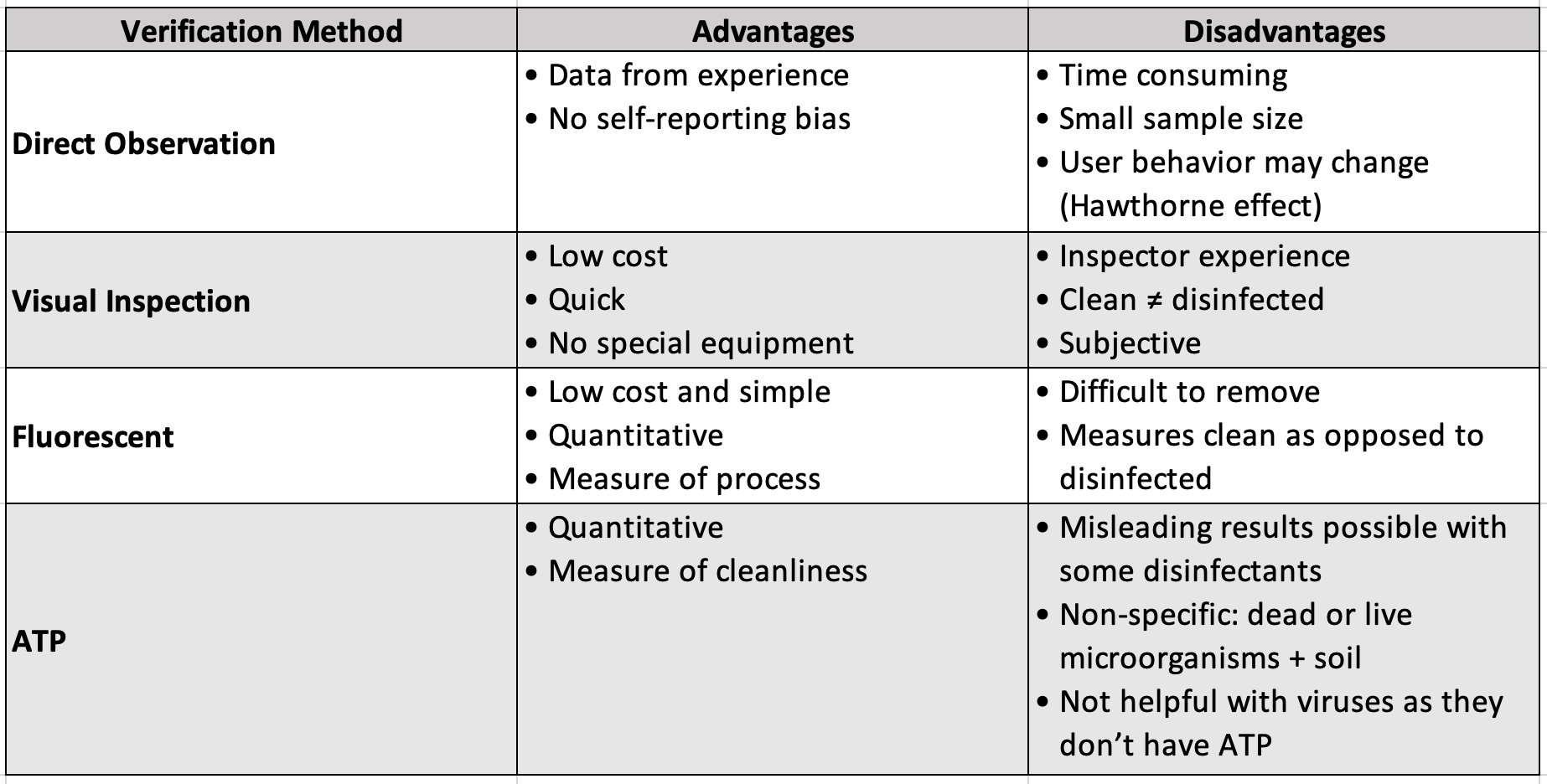
According to the CDC, cleaning procedures should be periodically monitored or assessed to ensure they are consistently and correctly performed4. Monitor cleaning and disinfection by employing various methods of verification including direct observation, visual inspection, use of fluorescent gel, and adenosine triphosphate (ATP) testing. Each of these methods has advantages and disadvantages as shown in Table 1, so it is important to implement several based on the needs of the facility.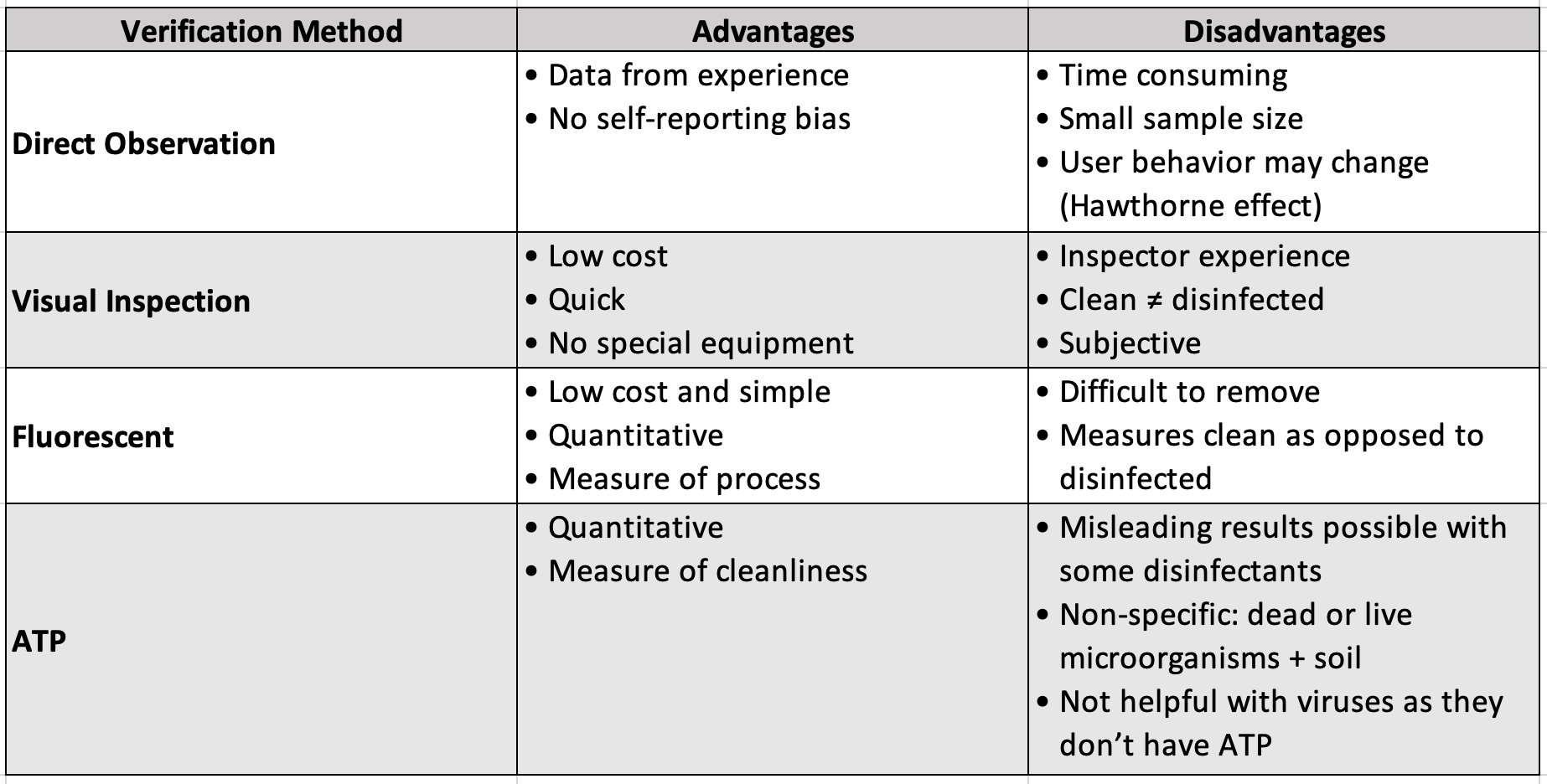
-
Process Improvement
After gaining a better understanding of the gaps and breakdowns in cleaning and disinfection, process improvement can begin. This should involve reevaluating goals and objectives, pinpointing deficiencies, and then responding by developing a plan and implementing a program or intervention to address any issues. Increased compliance and a robust program will result from ongoing process improvement.
These strategies are key to a successful environmental cleaning and disinfection program. By refocusing on the basics of environmental cleaning and disinfection, healthcare facilities will be able to remain steadfast in providing healthy and safe environments for patients while reducing the risk of HAIs despite current and future challenges.
For more on cleaning and disinfection basics, be sure to view the webinar Bringing it Back to the Basics — Cleaning and Disinfection Tidbits I Wish I’d Known as a Novice IP, part one of the three-part series: Cleaning & Disinfection — From Basics to Innovation.
References
^1. CMS State Operations Manual, Appendix A, 2018 [internet]. Available from https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/som107ap_a_hospitals.pdf.
2. Schaefer MK, Jhung M, Dahl M, Schillie S, Simpson C, Llata E, et al. Infection control assessment of ambulatory surgical centers. JAMA. 2010;303(22):2273–9
3. Furlan MCR, Ferreira AM, da Silva Barcelos L, Rigotti MA, de Sousa AFL, Dos Santos Junior AG, et al. Evaluation of disinfection of surfaces at an outpatient unit before and after an intervention program. BMC Infect Dis. 2019;19(1):355.
4. Centers for Disease Control and Prevention. Guide to Infection Prevention for Outpatient Settings: Minimum Expectations for Safe Care. http://www.cdc.gov/HAI/settings/outpatient/outpatient-care-guidelines.html.^