Understanding MDRO Susceptibility to Disinfectants: Insights for Infection Prevention
As antimicrobial resistance (AMR) continues to be a critical issue in both clinical and public health settings, one question we hear often from infection preventionists (IPs) is whether multidrug resistant organisms (MDROs) are harder to kill on surfaces.
The short answer: drug resistance does not automatically translate to disinfectant resistance. Our 2025 commentary in the American Journal of Infection Control (AJIC) aims to explain why and what that means for product selection and IPC practice.

When pathogens evolve faster than product labels
The increasing prevalence of AMR pathogens has led to a perceived need that a healthcare disinfectant must have an Environmental Protection Agency (EPA)-registered pathogen kill claim against every AMR pathogen of concern.
Currently, the EPA only has a product use policy for emerging viral pathogens but does not yet have a policy for emerging bacterial pathogens to allow product use for similar types of bacteria. This creates significant challenges as multi-drug resistance organisms (MDROs) continue to evolve and regulatory updates to registered products can take several years from testing to updated in-market product labels. Often, by the time a new pathogen is tested and added to an EPA-registered product, the MDRO has evolved to have increased resistance not captured by the original strain tested for susceptibility.
Through all of this, healthcare facilities are left wondering whether their current disinfectants are providing the right level of efficacy to kill the most current resistant threats.
Why drug resistance and disinfectant resistance differ
To be effective, antibiotics must maintain safety profiles for systemic human administration and function within the constraints of minimum inhibitory concentrations (MICs) and act on specific molecular targets, such as protein synthesis or cell wall formation. Due to the fact that they rely on precise mechanisms, even small genetic changes in bacteria can create resistance. In contrast, EPA registered surface disinfectants are used at concentrations far above MICs and typically act through multiple, nonspecific mechanisms all at once (e.g., protein denaturation, membrane disruption, oxidation). Consequently, marginal increases in microbial resistance, which critically impact antimicrobial drug efficacy, are highly unlikely to affect disinfectant performance.1
That said, disinfectant resistance development can occur under suboptimal conditions, wherein disinfectant concentrations fall below effective thresholds. Such scenarios may result from:
- Improper dilution as seen with dilutable disinfectants2
- Inadequate application practices
- Failure to adhere to manufacturer-specified contact times
- Use of non-EPA-registered formulations
One of the best ways to ensure disinfectants are maintained at the proper concentration is to utilize ready-to-use (RTU) disinfectants and adhere to directions-for-use (DFUs) on the product label.
What our testing reveals about MDRO susceptibility to disinfection
In our review of Good Laboratory Practice (GLP) testing across seven healthcare disinfectants (including bleach, hydrogen peroxide, and quat based formulations), we compared wild type strains with their antibiotic resistant counterparts (e.g., MRSA vs. S. aureus, VRE vs. E. faecalis, ESBL/NDM 1 E. coli and K. pneumoniae). Across 55 paired results, efficacy was consistent between wild type and resistant strains when disinfectants were used as labeled. Our findings indicate that when a disinfectant holds an EPA-registered efficacy claim for one strain of a given bacterium, the absence of a specific claim for another antimicrobial-resistant variant does not imply diminished effectiveness against it.
For a practical, shareable overview, see our study summary, Antibiotic Resistance Does Not Equate to Disinfectant Resistance.
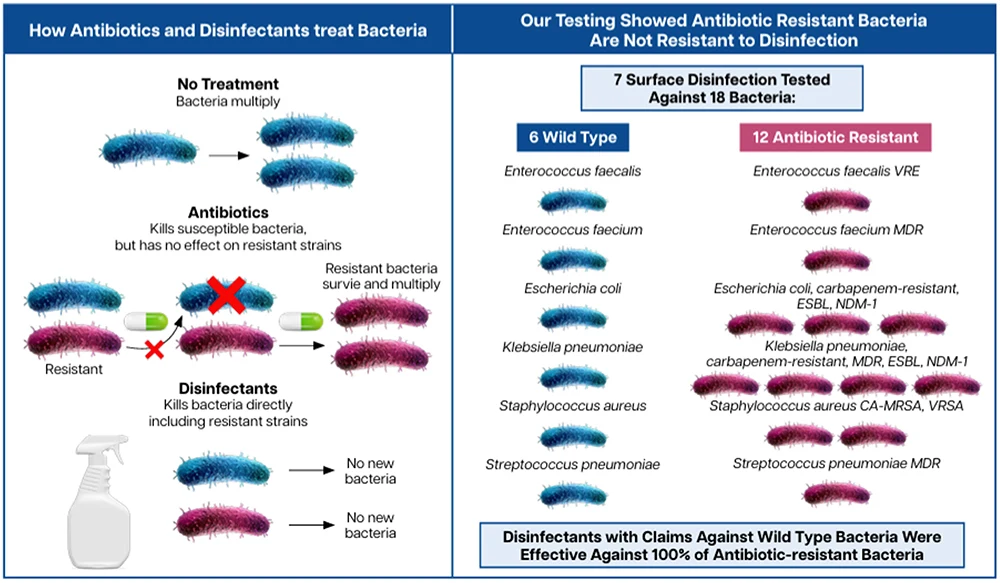
As antibiotic resistance continues to rise, disinfectants remain one of the most effective tools for reducing MDRO transmission in the healthcare environment. Unlike antibiotics, which face growing resistance pressures, EPA‑registered disinfectants used at proper concentrations remain highly effective at killing both susceptible and resistant strains on surfaces.
RTU formulations offer a dependable solution that supports compliance, eliminates dilution variability, and ensures that disinfectants are always used at the right concentration. Looking ahead, the strategic use of RTU disinfectants will be essential in helping facilities stay ahead of emerging resistance threats.
Share this article
More from the Clorox Pro Blog
References
- Rozman U, Pušnik M, Kmetec S, Duh D, Šostar Turk S. Reduced susceptibility and increased resistance of bacteria against disinfectants: a systematic review. Microorganisms [Internet]. 2021 [cited 2026 Jan 2];9(12):2550. Available from: https://doi.org/10.3390/microorganisms9122550
- Cadnum JL, Kaple CE, Eckstein EC, et al. Dilution dysfunction: evaluation of automated disinfectant dispenser systems in 10 hospitals demonstrates a need for improved monitoring to ensure that correct disinfectant concentrations are delivered. Infect Control Hosp Epidemiol [Internet]. 2024 Oct 10 [cited 2026 Jan 2]. Available from: https://doi.org/10.1017/ice.2024.148














