Is Pathogen Resistance to Disinfectants Fact or Fiction?

Antibiotic resistance remains a grave concern in the healthcare industry and public health, in general. Antibiotics and antifungals (both types of antimicrobials) can save lives, but any time they are used, they can contribute to resistance. Per the Centers for Disease Control and Prevention’s (CDC) 2022 Special Report: COVID-19 U.S. Impact on Antimicrobial Resistance, resistant hospital-onset infections and deaths both increased at least 15% during the first year of the COVID-19 pandemic.1 In a 2021 analysis, the CDC also reported that, after years of steady reductions in healthcare-associated infections (HAIs), U.S. hospitals saw significantly higher rates for four out of six types of HAIs in 2020. Many of these HAIs are resistant to antibiotics or antifungals.2 In fact, six out of 18 of the most concerning antimicrobial resistance pathogens cost the U.S. more than $4.6 billion annually.3
As our attention is increasingly on antibiotic resistance organisms, many in the professional cleaning space have begun to wonder whether pathogens can also develop resistance to chemical disinfectants. However, confusion around this question naturally develops as there are actually two types of pathogen resistance:
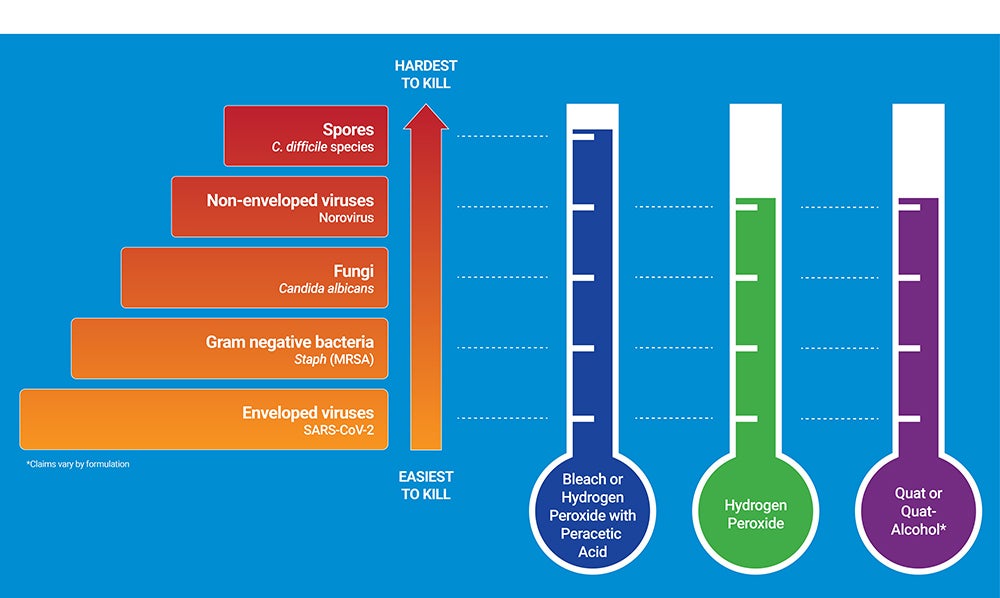
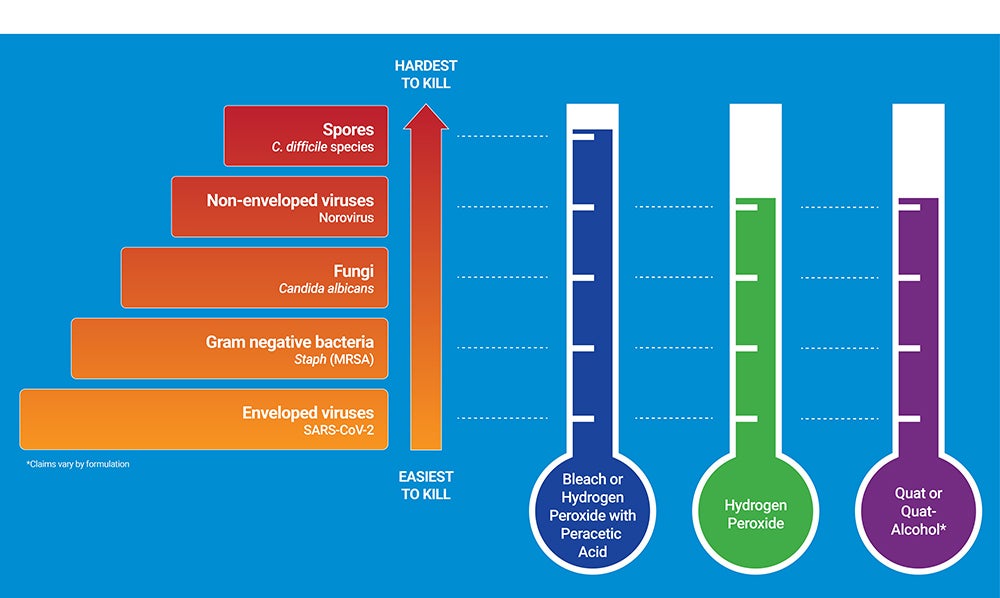
-
Innate resistance - Pathogens vary greatly in their natural resistance or susceptibility to antimicrobials and chemical disinfectants (i.e., how easily are they killed by antimicrobials or disinfectants). For example, spores are highly resistant to disinfectants and therefore hardest to kill because of their spore coat and outer shell, which act as a natural barrier. This is not something that is acquired or changing over time. The pathogen hierarchy chart below helps to demonstrate the innate resistance of varying pathogens to the various chemical disinfectants available today.
-
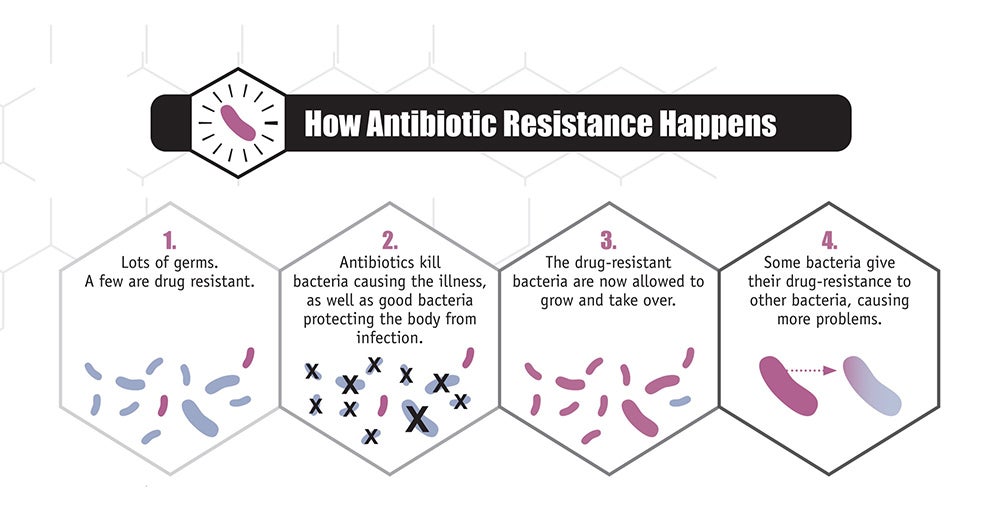
Acquired resistance - Acquired resistance happens when pathogens, like bacteria and fungi, develop the ability to defeat the drugs designed to kill them. This often happens due to the selective pressure that occurs when antimicrobials are used to kill germs that cause infections, but they fail to kill all of the remaining pathogens because some have natural immunity.4 The antimicrobial-resistant germs survive and multiply.
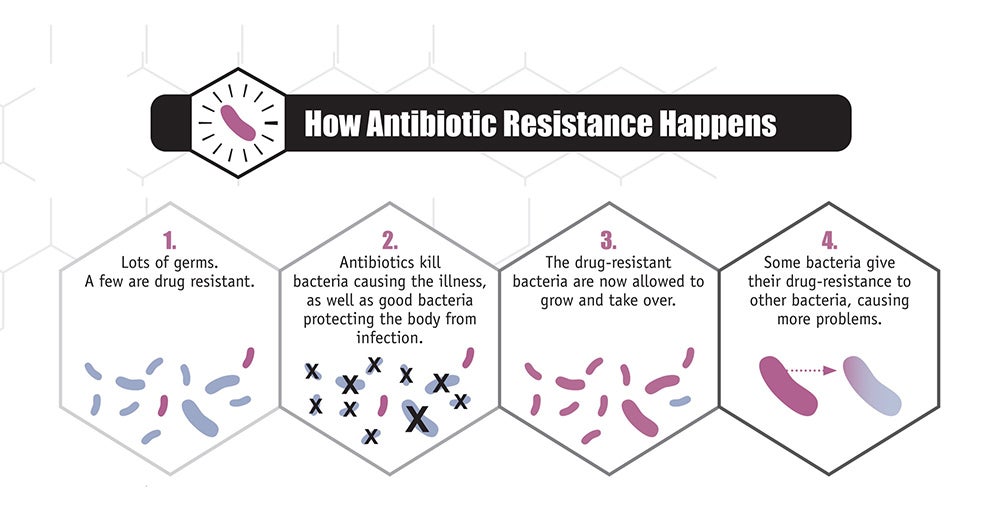
@2013 CDC/ Antibiotic Resistance Coordination and Strategy Unit
So, can pathogens also acquire resistance to disinfectants?
The simple answer is yes; disinfectants have been shown to impart selective pressure on some types of bacteria resulting in the development of acquired resistance.5,6,7 However, bacteria are only capable of developing resistance to certain types of disinfectants if the concentration of the active ingredient is too low to be efficacious. This can sometimes occur from the use of unregulated products in the marketplace, human error while mixing, storing, and handling dilutable disinfectants, or when the product label directions for use are not followed correctly (contact time, expiry date, etc.).8,9,10
Though research on disinfectant resistance is ongoing, one thing is clear: pathogens do not become resistant to disinfectants or germicides in the same way they do to antimicrobials. Notable differences include, but are not limited to:
- Disinfectants have multiple ways of attacking pathogens.11 In fact, the method of kill is entirely dependent on the active ingredient(s) and how they are formulated. In general, disinfectants can denature, oxidize, or attack pathogens in various ways.
- Disinfectants are used on inanimate surfaces rather than inside the body. By contrast, antimicrobials are used inside the body and therefore have limitations on the overall concentration that can be used safely inside a human body. This allows disinfectants to be used at concentrations that far and away exceed the required minimum kill concentration (known as the minimum inhibitory concentration). Therefore, a small increase in resistance, while critically important to an antimicrobial, would be of little relevance to the effectiveness of a disinfectant.
In general, as long as a facility is using a good quality, U.S. Environmental Protection Agency-registered disinfectant and they are using it correctly, there should be no concerns of disinfectant resistance. Disinfectants are one of the most viable protections against multi-drug resistant organisms (MDROs) and disinfectants could play an increasingly important role in managing bacterial infections in the future if the current trend of antibiotic resistance continues.1
References
^1. 2022 Special Report: COVID-19 U.S. Impact on Antimicrobial Resistance. Centers for Disease Control and Prevention. 2022 [Cited October 1, 2022]. Available From: https://www.cdc.gov/drugresistance/pdf/covid19-impact-report-508.pdf
2. Current HAI Progress Report: 2020 National and State Healthcare-Associated Infections Progress Report [Internet]. Centers for Disease Control and Prevention. 2021 [Cited October 1, 2022]. Available From: https://www.cdc.gov/hai/data/portal/progress-report.html
3. Nelson RE, Hatfield KM, Wolford H, Samore MH, Scott RD, Reddy SC, et al. National Estimates of Healthcare Costs Associated With Multidrug-Resistant Bacterial Infections Among Hospitalized Patients in the United States. Clin Infect Dis [Internet]. 2021 Jan 15 [Cited October 1, 2022];72(Suppl 1):S17–26. Available from: https://pubmed.ncbi.nlm.nih.gov/33512523/
4. Antimicrobial Resistance: How Antimicrobial Resistance Happens. Centers for Disease Control and Prevention. 2021 [Cited October 1, 2022]. Available From: https://www.cdc.gov/drugresistance/about/how-resistance-happens.html
5. Rozman U, Pušnik M, Kmetec S, Duh D, Turk SŠ. Reduced Susceptibility and Increased Resistance of Bacteria against Disinfectants: A Systematic Review. Microorganisms [Internet]. 2021 Dec 1 [Cited October 1, 2022];9(12). Available from: /pmc/articles/PMC8706950/
6. Mc Carlie S, Boucher CE, Bragg RR. Molecular basis of bacterial disinfectant resistance. Drug Resist Update [Internet]. 2020 Jan 1 [Cited October 1, 2022];48. Available from: https://pubmed.ncbi.nlm.nih.gov/31830738/
7. Boyce JM, Havill NL. In-use contamination of a hospital-grade disinfectant. Am J Infect Control [Internet]. 2022 [Cited October 1, 2022];0(0). Available from: http://www.ajicjournal.org/article/S0196655322001481/fulltext
8. Harbarth S, Tuan Soh S, Horner C, Wilcox MH. Is reduced susceptibility to disinfectants and antiseptics a risk in healthcare settings? A point/counterpoint review. J Hosp Infect [Internet]. 2014 [Cited October 1, 2022];87(4):194–202. Available from: https://pubmed.ncbi.nlm.nih.gov/24996517/
9. Sheldon AT. Antiseptic “resistance”: real or perceived threat? Clin Infect Dis [Internet]. 2005 Jun 1 [Cited October 1, 2022];40(11):1650–6. Available from: https://pubmed.ncbi.nlm.nih.gov/15889364/
10. Bragg R, Jansen A, Coetzee M, van der westhuizen W, Boucher C. Bacterial resistance to Quaternary Ammonium Compounds (QAC) disinfectants. Adv Exp Med Biol [Internet]. 2014 [Cited October 1, 2022];808:1–13. Available from: https://pubmed.ncbi.nlm.nih.gov/24595606/
11. Weber DJ, Rutala WA. Use of germicides in the home and the healthcare setting: is there a relationship between germicide use and antibiotic resistance? Infect Control Hosp Epidemiol [Internet]. 2006 Oct [Cited October 1, 2022];27(10):1107–19. Available from: https://pubmed.ncbi.nlm.nih.gov/17006819/^