
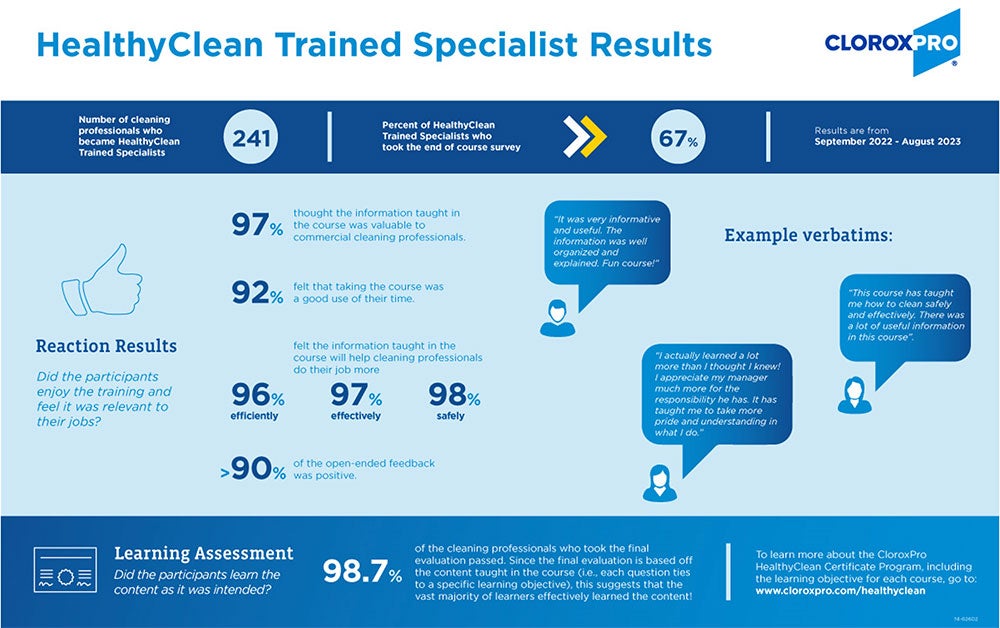
With almost 60% of in-house facility managers identifying training as a top issue, we know that training is crucial in the cleaning industry.1 However, it is very time consuming to create and execute on your own, and sometimes supplemental training is needed. Fortunately, there are many training options now available, but how do you know if they are worth your time? The good news is there is an established model of assessing training outcomes that can help!
In this blog, I will introduce you to the Kirkpatrick Model by covering 1) What it is, 2) How it can be used, and, 3) some of the results from the HealthyClean Certificate Program as an example. 2
Let's get started...
What is the Kirkpatrick model?
The Kirkpatrick model is a method of measuring learning effectiveness. It was developed in the 1950s by Don Kirkpatrick as part of his Ph.D. work at the University of Wisconsin. Since then, the model has become well established in the instructional design industry, becoming the leading model to assess if learning outcomes have been achieved .3
The Kirkpatrick model uses four levels to assess learning. The levels begin with the basics (did participants enjoy the course?) and move to bigger impacts of the training (did the training positively impact the business?). The table below outlines the four levels, what questions each seeks to answer, and the data used to answer each question.
| Level | Question | Data used |
| Participants Reaction | Did the participants enjoy the training and feel it was relevant to their job? | End of course survey that asks the learner what they felt about the training |
| Learning | Did the participants learn the content as was intended? | End of course evaluations (also called tests, quizzes, or assessments) |
| Behavior Change | Did the participants apply what they learned on the job? | Observation or survey after returning to work |
| Business Results | Were business outcomes achieved because of the training? | Pre-established Key Performance Indicators (KPIs). e.g., less complaints, turnover, or injuries |
Using the Kirkpatrick model
In an ideal world, all levels of the Kirkpatrick model would be assessed for all courses. In my experience, however, outcomes from any level are hard to come by. Time, money, resources, and knowing how to measure and what to ask for are barriers to understanding the true effectiveness of training programs. But, in an era where training is of utmost importance, and where everyone is stretched for time, assessing training for effectiveness and impact is one of the best things we can do to make sure we are using our time wisely.
So how can you use the information above to determine if a course is worth your time? Here are three suggestions:
- Review the training's learning objectives and ensure they meet your staff's learning needs.
- It’s a hard stop if the learning objectives don’t set out to train on what your employee's needs.
- The training should also test the learner on each learning objective to ensure they learned the information. A good rule of thumb is one question per learning objective, but there may be more.
- Ask the course developer for the outcomes of the training.
- Use the table above to help explain what questions you are looking to answer and understand the data they provide.
- Only move forward if you like the results, or if you are satisfied with the information that was provided.
- Pilot test with a few employees and do your own assessment.
- Participant Reaction: Ask your pilot group these questions:
- Did they like the training?
- Did they learn valuable information that will help them in their job?
- Did they think the training was a good use of their time?
- Learning: Ask your pilot group what they learned and see if it matches the stated learning objectives
- Behavior Change: Monitor to see if those in your pilot group apply the learnings from the training.
- Business Results: Keep track of KPIs that are important to your organization to see if there are larger business impacts after the pilot team took the training.
- Participant Reaction: Ask your pilot group these questions:
HealthyClean Results
If you’ve been following the CloroxPro journey into the world of high-quality education and training, you know that we now offer two ANSI-National Accreditation Board courses, and that to obtain those accreditations, we follow a global standard for measuring training outcomes.4
But what you may not know is that the ASTM standard requires certificate issuers to use an established model like Kirkpatrick's to monitor Participant Reaction and Learning. The goal of doing so is to drive continuous improvement, which is one of the ways that the training delivers quality over time.
As a result, CloroxPro has been doing yearly evaluations on the HealthyClean Trained Specialist Course since its launch in 2021. Below are some results from last year’s assessment.5 As time goes on, CloroxPro plans to expand to also include Behavior Change and Business Outcomes, so keep an eye on this space for more outcomes.
In conclusion, while most cleaning professionals recognize the importance of training, it is difficult to know which are worth their time. Fortunately, there are well established models like the Kirkpatrick Model that can help.
In this blog, I shared what the Kirkpatrick model is, how it helps with determining the value of a training, and some results from the HealthyClean Certificate Program as an example of how CloroxPro is putting the model to work for their own program.
To learn more about high quality education & training, check out my other blogs:
- Three C’s of Credibility
- Why Instructional Design Matters
- The ABCs of Credentialing
- Help Is Here! Becoming a Successful “Cleaning for Health” Manager
References
1. 2023 CMM In-House/Facility Management Benchmarking Survey Report [Internet]. Cleaning & Maintenance Management. Available from: https://cmmonline.com/articles/2023-cmm-in-house-facility-management-benchmarking-survey-report
2. Kirkpatrick DL. The Four Levels of Evaluation. Evaluating Corporate Training: Models and Issues. 1998; 46:95–112.
3. Kirkpatrick Partners | About Us | Donald L. Kirkpatrick, PhD [Internet]. Kirkpatrick Partners, LLC. Available from: https://www.kirkpatrickpartners.com/about-us/don-kirkpatrick/
4. Standard Practice for Certificate Programs [Internet]. www.astm.org. [cited 2024 Feb 13]. Available from: https://www.astm.org/e2659-18.html
5. Strazdas L and Rops, M. 2023; CloroxPro HealthyClean 2023 Program Evaluation
With 90% of companies requiring a return-to-office (RTO) by 2024, the demand for cleaning for health has never been higher.1 In fact, a recent survey of facility executives found that 40% would pay a higher price for "increased infection control procedures."2 With increased awareness of germs, our cleaning staff is under more pressure than ever before. But here's the catch: the turnover rate is soaring, and many are cleaning without proper training.3 This scenario has left our cleaning managers juggling a daunting array of tasks, leading to exhaustion and burnout.
In this blog, I'll shed light on crucial aspects that cleaning for health managers must grasp for success. This includes understanding what cleaning for health is, becoming familiar with best practices, and mastering the art of management that are important with these practices. While I aim to offer valuable information here, the realm of knowledge extends far beyond this scope. If you're eager to dive deeper, I encourage you to explore the wealth of information available in the new ANSI National Accreditation Board-accredited HealthyClean® Trained Manager Certificate Course generously offered for free by CloroxPro. Seize this opportunity today and enhance your expertise and credibility in the world of cleaning for health with this brand-new program! More information is available below.
Decoding Cleaning for Health
Cleaning for health is the process of maintaining and keeping buildings visibly clean and reducing the spread of germs and other unwanted matter.3 To clean for health requires specific approaches, best practices and tools that are focused on removing unwanted matter from a building that has the potential to impact health. While it should be the goal of every cleaning operation, due to its complexity and differences in how it needs to get done, that is not always the case. At the onset, cleaning for health appears to place additional demands on an operation, but in fact, it can be incorporated and even lead to reductions in time and labor when implemented properly.
3 Cleaning for Health Cleaning Essentials for Managers
- Cleaning and disinfecting can help break the chain of infection: One way that germs spread from person to person is through inanimate objects like door handles, light switches, and elevator buttons. When done properly, cleaning can interrupt the spread by killing germs on surfaces so that they cannot spread. Conversely, cleaning improperly can have the opposite effect, by cross-contaminating in the indoor environment.
- Safe techniques help avoid injury: Lifting with your legs and not your back, mopping 2–3 feet in front of you, not overloading your cart, and asking for help if when lifting heavy items are all things that front-line cleaners can do to help stay safe while working.
- Ready-to-use (RTU) products are efficient, effective, and safe: Not having to prepare a product prior to a shift or going back to the supply closet to refill offers an efficiency that is not often considered when purchasing a product. RTU products are always at the right concentration to work as intended. With RTUs, there is no opportunity to under dilute, which can create a more toxic product, or overdilute, which could cause the product to be ineffective. Frontline cleaners prefer to use RTU products because they know they work, and products that work lead to more efficient operations.
3 Cleaning for Health Managing Essentials for Managers
- Communication is king: Whether it be with front line cleaners or building owners, communication is critical to helping the operation run smoothly. Lack of clear communication leads to lack of appreciation and can also lead to confusion and distrust.
- Standardization keeps it simple: Standardization is using the same equipment, tools, materials, products, and processes across an organization. It makes logistics, purchasing, training, and auditing simpler and more efficient. Using the same products across an organization, color coding clothes, and kitting janitor supplies and tools are examples of standardization.
- Training engages and improves outcomes: When employees feel invested in performance improves, buildings are healthier, and turnover declines.
In the face of increased demands and heightened awareness surrounding hygiene, the role of cleaning for health managers has never been more crucial. As frontline cleaners navigate this challenge, the strain on managers is real too. In this blog, I've explored essential elements of cleaning for health, shedding light on what it is, best practices, and how management’s role is essential. While it provides some foundational understanding, the world of expertise in cleaning for health is much broader than this. To further improve your knowledge and skills, I encourage you to take advantage of the new opportunity offered by CloroxPro's new Trained Manager course. More information is available below. Empower yourself today and embrace the path toward becoming a proficient and successful cleaning for health manager. Together, we can elevate our standards and create safer, healthier environments for all!
The CloroxPro HealthyClean Certificate Program offers high-quality and FREE education and training on Cleaning for Health for frontline cleaners & managers, including:
- NEW! An ANSI National Accreditation Board-accredited Trained Manager course on Cleaning for Health and designed for cleaning managers.
- An ANSI National Accreditation Board-accredited Trained Specialist course on Cleaning for Health and designed for front-line cleaners and managers (available in both English & Spanish)
- A 20 min microlearning module on cleaning and disinfecting in healthcare and designed for EVS managers.
- 3 short (5-7 min) microlearning modules addressing some of the most challenging commercial cleaning tasks designed for cleaning managers. These modules each introduce a CloroxPro product that can help.
Become a successful cleaning for health manager by supplementing your current program with ours today!
- To learn more or sign up, visit our website at www.cloroxpro.com/healthyclean
- To learn more about what high-quality education and training is, check out these blogs on finding the right education and training program:
References
1. Hyken S. Nine Out Of 10 Companies Will Require Employees To Return To The Office [Internet]. Forbes. [cited 2023 Oct 16]. Available from: https://www.forbes.com/sites/shephyken/2023/09/24/nine-out-of-10-companies-will-require-employees-to-return-to-the-office/?sh=56fd0ece2baf
2. Results: 2023 Facility Executive Contractor Expectations Survey [Internet]. CleanLink. [cited 2023 Oct 16]. Available from: https://www.cleanlink.com/cp/article/Results-2023-Facility-Executive-Contractor-Expectations-Survey--29867
3. Five Industrial & Institutional Cleaning Trends That Will Define 2023 - Kline & Company [Internet]. klinegroup.com. 2023 [cited 2023 Oct 16]. Available from: https://klinegroup.com/articles/five-industrial-and-institutional-cleaning-trends-that-will-define-2023/
4. Berry MA. Protecting the Built Environment: Cleaning for Health [Internet]. Amazon. Tricomm Twenty First Pr; 1994 [cited 2023 Oct 16]. Available from: https://www.amazon.com/Protecting-Built-Environment-Cleaning-Health/dp/0963571508
We all know too much grease in our diet isn’t good for us, and the same holds true for grease in buildings. It can create slippery surfaces that lead to falls1,2, and if left untreated, can build up into grimy areas that harbor bacteria and odors (or even catch on fire!). Grease can get down drains and cause pipes to clog, back up, and break, which can lead to flooding and sewage contamination. And in machinery maintenance areas, oil and grease leaks can cause engines to come to a grinding halt and leave unprotected surfaces stained and unsightly. For these reasons and more, I will cover what cleaning managers and supervisors should know about grease and grime on surfaces, and what can be done to save you from potential headaches down the line.
What are grease & grime?
According to Cambridge Dictionary, grease is animal or vegetable fat that is soft after melting, or more generally, any thick oil-like substance.3 Grime, is even worse. It is what happens when oil or grease combines with other soils like dirt, soot and becomes hard. Over time, grime can become embedded and/or strongly stuck to a surface, making it difficult to remove. Imagine grease as the splatter on a stovetop immediately after frying and grime as what is on the top of a nearby ceiling fan weeks later.
What causes grease & grime?
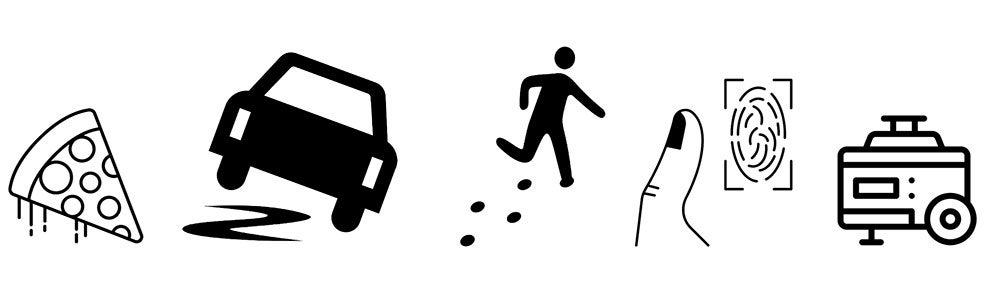
Even when grease and grime aren’t causing major disruptions, they can still give rise to everyday inconveniences. For example, grease and grime can emit unpleasant odors, unsightly appearances, and provide a food source for germs. Beyond the large amounts of grease associated with cooking and food preparation activities, it’s interesting to consider the other sources of grease within a facility come from. Here are some less obvious origins that may catch you by surprise.
- Fast Food: Approximately 37% or 50 million Americans consume fast food on any given day, including while they are at work.4
- Our Skin: Our skin produces oil to help keep our skin soft and smooth and protect us from absorbing too much water when we get wet.5 This means that along with spreading germs, our fingers are also good at spreading oil and grease.
- Tracked in on Shoes: Motor oil and grease can be tracked in from parking lots, where leaky cars drip oil, or in maintenance areas where machinery and devices are cleaned and repaired.
- Backup Generators: As the need for backup systems increases due to power outages or other emergencies, so does the need for oil in a facility, which is required for a generator to run.6
Tackling grease & grime
Addressing both obvious and unexpected sources of grease and grime is important for maintaining a clean and hygienic indoor environment. To begin, identify where grease can show up in your facility. Look in places like kitchens, dining areas, floors near kitchen areas, and places people touch a lot like handrails, door handles, keyboards, light figures, and elevator buttons. Also don’t’ forget about maintenance areas. Once you know where it is, follow these other tips to keep it under control.
- Clean Regularly: Tackle grease and grime on a daily or weekly basis. This will ensure they don’t build up and cause major issues.
- Use Effective Products: Invest in a product that is formulated to remove grease and grime and kill odor-causing bacteria. Products that are specially formulated to address grease and grime can help cut down on the labor needed to do the work, potentially saving time, and reducing the amount of effort needed by frontline staff to get the job done.
- Promote Reduction: Encourage facilities to use less. Cutting back on the amount used will not only make cleaning easier, but when it comes to the food consumed, it will be better for human health too.
- Protect the Pipes: Regularly maintain grease traps and use a disposable wipe or cloth. These steps will keep grease and grime from getting into the sewer system, where it can block pipes and cause backups.7,8 According to the EPA, restaurants can product and contribute between 800 to 17,000 pounds of grease waste to sewage treatment plants each year.9
- Be Ready for Spills: Have a kit that contains PPE, disposable bags, absorbent material, and a product that is effective. Train staff to be able to effectively, safely, and efficiently clean up a oil or grease spill if one should occur.
“It is better to prepare and prevent than it is to repair and repent.”
Ezra Taft Benson
Conclusion
Grease is commonly associated with cooking and something we all know to avoid as part of our regular diets (whether we do or not is a topic for another blog!). When combined with other soils and present on surfaces, however, it can cause major problems in buildings too. With a better understanding of what grease and grime are, where they come from, and best practices on how to tackle them, these issues can be avoided. In the wise words of Ezra Taft Benson, “It is better to prepare and prevent than it is to repair and repent” and it applies to grease and grime as well. Don’t let them slip you up!
References
1. Bitzas S, Ma S, Pesanelli K, Zaia AM. Risk factors and impacts of slips, trips, and falls in janitorial populations: A literature review. Appl Ergon. [Internet].2022;102. [cited 2023 Sept 25] Available from: https://pubmed.ncbi.nlm.nih.gov/35427905/
2. Centers for Disease Control and Prevention – The National Institute for Occupational Safety and Health (NIOSH).
Slip-resistant shoes reduce food services worker slip injuries [Internet]. [cited 2023 Sep 25]. Available from: https://www.cdc.gov/niosh/topics/falls/pdfs/Kitchen-Fnl_508.pdf
3. Cambridge Dictionary. grease [Internet]. @CambridgeWords. 2023 [cited 2023 Sep 25]. Available from: https://dictionary.cambridge.org/us/dictionary/english/grease
4. Fryar C, Hughes J, Herrick K, Ahluwalia N. Centers for Disease Control & Prevention. Fast Food Consumption Among Adults in the United States, 2013–2016. Products - Data Briefs - Number 320 - September 2018 [Internet]. CDC. 2018. Available from: https://www.cdc.gov/nchs/products/databriefs/db322.htm
5. Cleveland Clinic. An Overview of Your Skin | Cleveland Clinic [Internet]. Cleveland Clinic. 2021. Available from: https://my.clevelandclinic.org/health/articles/10978-skin
6. Maintenance Tips for Your Facility’s Backup Power Generator [Internet]. Facilities Management Advisor. 2023 [cited 2023 Sep 25]. Available from: https://facilitiesmanagementadvisor.blr.com/emergency-preparedness/maintenance-tips-for-your-facilitys-backup-power-generator/
7. OSHA Hazard Bulletin. Grease Trap Hazards [Internet]. Available from: https://www.osha.gov/sites/default/files/publications/OSHA3986.pdf
8. O’Shields SM.. F.O.G. (Fats, Oils, and Grease) Polluion [Internet]. Clemson Cooperative Extension. 2019 [cited 2023 Sept 25] Available from: https://hgic.clemson.edu/factsheet/f-o-g-fats-oils-and-grease-pollution/
9. EPA National Pretreatment Program. Controlling Fats, Oils, and Grease Discharges from Food Service Establishments 2012 [cited 2023 Sept 25] Available from: https://www3.epa.gov/npdes/pubs/pretreatment_foodservice_fs.pdf

It’s a fact: Education and training leads to many positive outcomes in today’s workforce, including increased productivity, reduced turnover, and improved outcomes.1,2 I was reminded of this recently when I attended the Association for Talent Development’s annual conference (ATD23), which brought together over 10,000 attendees and 300 vendors from 50 countries, united in the vision of “creating a world that works better”. Yet, while the value of education and training are clearly understood by many, an excuse I hear often in the cleaning industry is that there is not time for it. This couldn’t be further from the truth. If you are a cleaning manager or supervisor and you are not prioritizing the education and training of your staff, you are missing out on a huge opportunity to benefit your business and organization by unlocking the full potential of your staff. Henry Ford said it well when he said, “The only thing worse than training your employees and having them leave, is NOT training them and having them stay.”
"Creating a world that works better"
Still not convinced?
In this blog, I’ll dive into some of the most recent peer-reviewed evidence that highlights the positive impact of education and training programs on cleaning operations. These studies are from healthcare, but the results can be applied to any setting. This is because many cleaning-for-health best practices are similar across building types. For example, front-line cleaners both in and outside of healthcare should be thoroughly cleaning the surfaces they have been assigned, they should always wipe in an s-shape pattern, and when disinfecting, they should always ensure the product stays wet for the contact time. I hope these studies, along with what the over 10,000 ATD23 attendees understand, will help you to find the time to educate and train your staff so that you can reap the many benefits as well.
“The only thing worse than training your employees and having them leave, is NOT training them and having them stay.”
Recent Published Studies
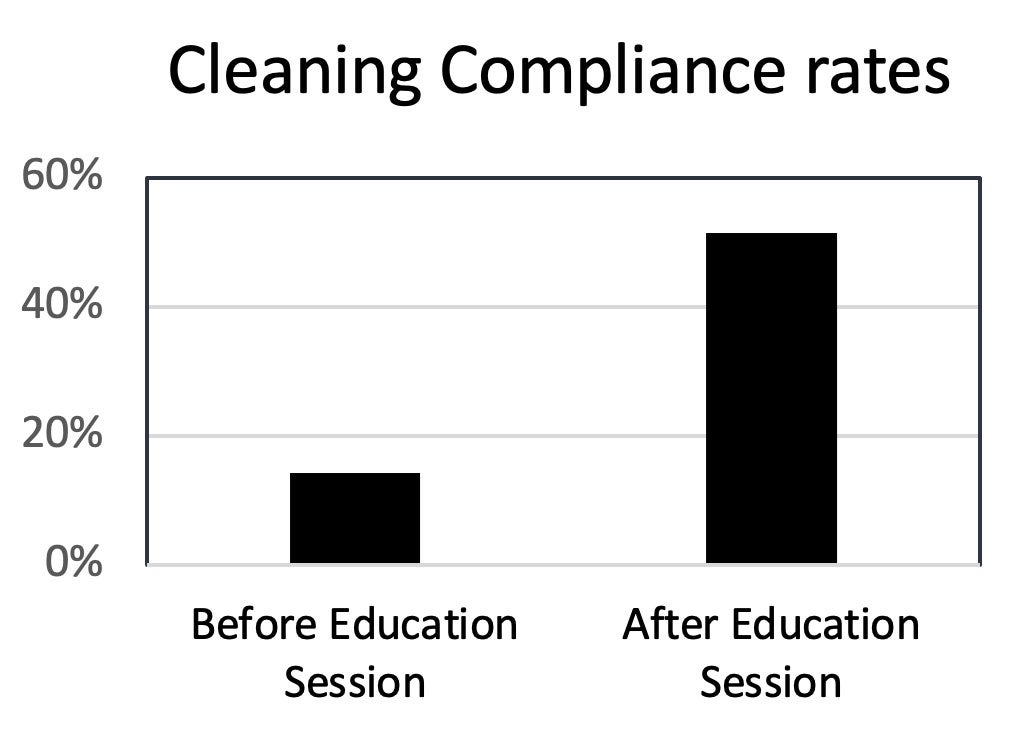
Study #1: An educational feedback session3
In this study, researchers examined how education can improve cleaning compliance in a healthcare setting. They used a fluorescent marker to assess if cleaning occurred on 700 surfaces in 35 inpatient rooms.
This study had three phases: a baseline assessment, an educational feedback session, and post-feedback assessment. They analyzed 350 surfaces in each assessment phase to measure compliance with cleaning and disinfection protocols.
Initially, during the baseline assessment, the compliance rate was low at 14.3%. This indicated inconsistent disinfection practices. After implementing the educational initiative and providing feedback, the compliance rate significantly increased to 51.4% in the post feedback phase.
Study #2: Education and training as part of structured system4
In this study, the hospital implemented a multi-pronged approach of education, training, monitoring, and feedback for the environmental services (i.e., healthcare cleaning operations, EVS) and infection prevention departments. The goal was to improve the cleaning practices and reduce the risk of infections in the healthcare setting.
To measure the effectiveness of this process, the researchers compared the cleaning performance before and after the implementation. Initially, the surface cleaning performance was at 74%. However, after the training program, the performance increased significantly to 90%, and it maintained at that level.
The positive impact of the training program was not limited to improved cleaning performance. The study also found that rates of C. diff infections decreased by 75%, indicating a significant reduction in the spread of this harmful bacteria.
Study #3: Special education sessions5
In this study, researchers examined 574 different surfaces in a dental school, over a period of three months. They also used a fluorescent marker to mark these surfaces. The purpose was to monitor how well these surfaces were being cleaned.
After the initial three-month period, the researchers shared their findings with the dental students, staff, and cleaning personnel during special education sessions. These sessions aimed to emphasize the importance of cleaning and disinfecting to prevent cross-contamination (the spread or transfer of germs from one area, surface, or person to another).
Following the educational sessions, the researchers continued their study for an additional three months. They re-examined 662 surfaces using the same method and the results were significant. They found statistically significant improvements in the cleanliness of the students’ dental cubicles, students’ x-ray areas, and elevator buttons, compared to their initial findings.

Surfaces with a statistically significant improvement in cleanliness after educational sessions
Conclusion
In conclusion, the ATD23 conference served as a powerful reminder of the value placed on education and training and it is clear from recent evidence that prioritizing education and training in the cleaning industry is also critically important. This is especially true as we are experiencing record levels of labor shortages and high turnover. With the emergency of the pandemic now behind us, I encourage you to act on the evidence and commit to making time for education and training for your staff. If you do, you will unlock their full potential, help ensure the continued success in your operation, and advance our important field.
Clorox Professional offers high-quality & FREE education and training, including:
- An ANSI National Accreditation Board-accredited training on Cleaning for Health and designed for frontline cleaners (available in both English & Spanish)
- A 20 min eLearning module on Cleaning and disinfecting in Healthcare and designed for EVS managers and supervisors.
- Several timely webinars, including Candida auris: An emerging threat in Long Term Care and Innovation in Green Cleaning, designed for Infection Preventionists and Cleaning Professionals both in and outside of healthcare.
Unlock your team’s potential by using our education & training to supplement your current programs!
To learn more or sign up, visit our website at www.cloroxpro.com/healthyclean and https://www.cloroxpro.com/educational-courses/
References
1. Arthur W. Jr., Bennett W. Jr., Edens, PS, Bell ST. Effectiveness of training in organizations: A meta-analysis of design and evaluation features. Journal of Applied Psychology [Internet].2003; 88(2), 234–245. [cited 2023 Jun 20] Available from: https://psycnet.apa.org/record/2003-03332-006
2. PwC. Navigating the rising tide of uncertainty. 23rd Annual Global CEO Survey [Internet]. 2020. [cited 2023 Jun 20] Available from: https://www.pwc.com/gx/en/ceo-survey/2020/reports/pwc-23rd-global-ceo-survey.pdf
3. Fram DS, Medeiros EA, Ribeiro RM, Escudero DVdS, Alves JCD, Macedo B, Ferreira DB, de Oliveira AHV, Santos RP, Matias LdO, Maia MM, Freires FJC, Ferreira VM, de Almeida TML, Machado FR. High-touch surfaces disinfection compliance in a COVID-19 intensive care unit. American Journal of Infection Control [Internet]. 2023; 51(4), 469–471. [cited 2023 Jun 20] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9444321/
4. Parry MF, Sestovic M, Renz C, Pangan A, Grant B, Shah AK. Environmental cleaning and disinfection: Sustaining changed practice and improving quality in the community hospital. Antimicrobial Stewardship & Healthcare Epidemiology [Internet]. 2022; 2(1), e113. Available from: http://pubmed.ncbi.nlm.nih.gov/36483421/
5. Dolev E, Eli I, Mashkit E, Grinberg N, Emodi-Perlman A. Fluorescent Marker as a Tool to Improve Strategies to Control Contaminated Surfaces and Decrease Danger of Cross-Contamination in Dental Clinics, during and beyond the COVID-19 Pandemic. International Journal of Environmental Research and Public Health [Internet]. 2023; 20(6), 5229. [cited 2023 Jun 26]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10049276/

Norovirus is a highly contagious virus that often causes outbreaks during the winter months, and this year has been no exception. From August 1, 2022, to February 12, 2023, NoroSTAT, a collaborative network of state health departments and the CDC, reported 254 norovirus outbreaks in participating states, including a multistate outbreak in Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, Tennessee, and Texas.1,2 Each norovirus outbreak can affect many individuals3, as seen in the several K-12 schools4,5 that have already been forced to shut down due to high numbers of norovirus cases this year.
As the norovirus season typically lasts until April, it is crucial to take preventive measures to help break the chain of infection.6 As a cleaning manager or supervisor, you also have an essential public health role in managing and preventing the spread of infections, including norovirus. While outbreaks can be stressful, there are several things you can do to help.
To assist you in managing the current norovirus outbreak, I have compiled a checklist of key questions with tips to follow. This guide will enable you to manage the situation effectively and easily, and by checking off each item, you will gain the confidence that you are helping to prevent and manage the spread of norovirus.
Key questions to answer during an outbreak
- What is the outbreak germ and how is it spread?
- The CDC is the best place to start learning about outbreak germs.3 Manufacturers often create relevant education material about outbreak germs too that can be useful.
- In the case of norovirus, it is a difficult to kill virus and it can spread easily from person to person in multiple ways.
- Importantly, it spreads easily from surfaces when an infected individual touches a surface contaminated with fecal or vomit particles with their bare hands or through the spattering of vomit or diarrhea onto surfaces. The virus can also be spread when tiny particles of vomit travel through the air and settle on surfaces or are ingested by another person.
- Are your building occupants and staff more susceptible to infection than the average population?
- Not everyone’s immune systems are created equal and there are some populations that are more susceptible to infections than others. In the case of norovirus, the young and elderly are the most vulnerable, and other susceptible populations include pregnant women, chemotherapy patients, and transplant recipients.
- If your building occupants, visitors, or staff are in any one of these categories, your role is even more important.
- Since only a few viral particles are needed to cause illness, it is a good idea to disinfect all shared surfaces, not just those “commonly touched”.
- Is your cleaning and disinfecting product EPA-registered to kill the outbreak germ?
- All disinfectants require EPA-registration in the United States, and products used against norovirus on surfaces should indicate this on the label. Because human norovirus is challenging to test in a laboratory environment, EPA-approved products have been tested against surrogate viruses, such as "feline calicivirus" or "murine norovirus," which are thought to be similar in how difficult they are to inactivate on an environmental surface.
- In addition to the EPA-registration against the outbreak germ, contact time is another attribute not to overlook. Look for products with low norovirus contact times to ensure efficacy (otherwise, your team may be wasting their time).
- While bleach-based products are often used for norovirus, do not assume that you must use them. If you look, you may be surprised to discover that even some eco conscious disinfectants have norovirus claims with short contact times!
- Do you need to increase the scope or frequency of cleaning and disinfecting in your facility?
- Review your facility risk assessment to help you make decisions on how to adjust your team’s work. Although many of the same daily tasks still need to be performed, surfaces that are usually lower risk may need to be cleaned and disinfected more often during the outbreak.
- If building occupants can help share some of the responsibility (beyond helping by washing their hands and staying home when sick), include the purchase of effective EPA-registered disinfecting wipes (with a norovirus claim of course) and place them in high-touch areas. Use signage to teach building occupants how to use products effectively and safely.
- Do you have enough product to effectively clean and disinfect during the outbreak?
- An easy way to do this is track the amount of product used during the first week of implementing your new protocols.
- Then, adjust the quantity ordered each time to accommodate the new volume.
- Do you need to provide staff with additional PPE based on how the outbreak germ spreads?
- Because norovirus can spread by surfaces and in some cases through the air (when someone nearby vomits), appropriate PPE to protect front line staff during a norovirus outbreak includes masks and gloves.
- When staff are introduced to new PPE, make sure they are trained on how to put it on, take it off, and wear it so it is effective while working.
- Does your staff need to be educated and trained on a new product and/or protocol?
- OSHA requires that staff are trained to use products safely and effectively. To do this, read the labels thoroughly and observe staff using the product correctly. Most manufacturers will offer directions for use product training to help free of charge.
- Be sure to document your training just in case you are asked to show the evidence during an inspection.
- It’s also a good time to assess and implement additional staff competency training.
- Do you have enough staff to address the additional frequency?
- It goes without saying that more work means that either something else must give, or more people are needed to do the job effectively and safely.
- An example tasks that may be put on hold during an outbreak are some deep cleaning or project work. Equipment maintenance tasks should never be postponed, however.
Congratulations you successfully managed the outbreak! Now what?
- Completing the norovirus outbreak checklist is a significant accomplishment, but do not keep it to yourself! Share it with upper management, staff, and building occupants to show them what your organization is doing to help keep them healthy and safe.
- While this outbreak may not last forever, another one is just around the corner. Save and bookmark this guide so you can use it again when you need it and, after the current outbreak is over, take the time to evaluate what worked and what didn't. This will help you make necessary adjustments and improvements for future outbreak management.
By taking these steps, learning from past experiences, and implementing the checklist, your team can be better equipped to help prevent and manage the spread of norovirus and other infections.
References
1. NoroSTAT Data [Internet] CDC. [cited 2023 March 9] Available from: https://www.cdc.gov/norovirus/reporting/norostat/data.html
2. Multistate Norovirus Outbreak Linked to Raw Oysters from Texas. [Internet] CDC. [cited 2023 March 6] Available from: https://www.cdc.gov/norovirus/outbreaks/index.html
3. About Norovirus [Internet] CDC. [cited 2023 March 9] Available from: https://www.cdc.gov/norovirus/about/index.html
4. Classes canceled at Livonia school following norovirus outbreak [Internet] The Detroit News [cited 2023 March 9] Available from: https://www.detroitnews.com/story/news/local/wayne-county/2023/02/11/classes-canceled-at-livonia-school-following-norovirus-outbreak/69895463007/
5. At Least 130 Sick in Norovirus Outbreak at Las Vegas School [Internet] The Food Poisoning Bulletin [cited 2023 March 9] Available from: https://foodpoisoningbulletin.com/2023/at-least-130-sick-in-norovirus-outbreak-at-las-vegas-school/
6. Norovirus Illness: Key facts. [Internet] CDC. [cited 2023 March 7] Available from: https://www.cdc.gov/norovirus/downloads/keyfacts.pdf
CloroxPro broke new ground when they launched the FIRST AND ONLY industry-wide training certificate course for commercial cleaners that is accredited by the ANSI National Accreditation Board (ANAB).1 To achieve this accreditation, they developed their online training course to meet over 130 requirements and went through a rigorous 3rd party review to confirm that their course met the ASTM E2659-18 standard.2 Receiving the ANAB-accreditation confirms the CloroxPro™ HealthyClean™ Trained Specialist Course provides high quality training and value to learners and raises the bar for education in the industry. It also means that employers can now be confident that the time spent on training will provide a return on their investment.
How do the requirements from ASTM E2659-18 lead to saving time?
Each requirement in the standard provides a framework for certificate courses to ensure optimal design, delivery, monitoring and learning outcomes. In short, the standard provides confidence that the training program does what it intends to do; and the learner gains the knowledge and skills outlined in the course. The 3rd party accreditation ensures the certificate holder has completed a high-quality course of study and they must pass a robust final evaluation to ensure learning objectives are met. Before the launch of the first version of the ASTM standard, there was no way to assess the quality of different certificate programs and if training was effective. The standard has since enabled “consumers, employers, government agencies, and others who rely upon a skilled workforce, to distinguish between qualified workers and those with fraudulent or less-than-quality credentials” — or worse, no credentials at all. For example, the standard requires that:
- Course development includes the use of evidence-based learning methods and best practices in instructional design.This means the curriculum is needed, that the learning process are engaging and effective, and there are measurable learning outcomes to confirm understanding of the training material.
- An external advisory panel guides course development. Subject matter experts representing the target learner provide input into the course’s learning objectives and design to ensure the curriculum and final evaluation will be appropriate and valuable in the profession.
- Management of the course follows predetermined processes, which include a mechanism for consistent feedback and ongoing quality improvement.
Are there other ways to ensure a course is high quality and therefore lead to saving time?
Yes, but only a few.
The ASTM E2659-18 standard is one of only two internationally recognized standards for certificate courses developed by ANSI approved Standard Developing Organizations (SDOs). It is also the only one that ANSI National Accreditation Board accredits against and the one with more accredited certificate courses.3 In addition to the CloroxPro™ HealthyClean™ Certificate Program, here are four other courses that are ANAB-accredited against ASTM E2659-18:
- National Restaurant Association — ServSafe Food Handler Program
- International Facility Management Association (IFMA) — Facility Management Professional (FMP)
- IFMA — Sustainability Facility Professional (SFP)
- Green Advantage — Pre-construction Risk Assessment – Infection Control Risk Assessment (PCRA/ICRA) Certificate Program
The Institute for Credentialing Excellent (ICE) accredits against the second standard, the ICE 1100:2019 - Standard for Assessment Based Certificate Programs.4 Three examples of certificate courses that are ICE-accredited5 include:
- American Association of Medical Assistants — Assessment-Based Certificate Program in Pediatrics
- International Hearing Society — Tinnitus Care Provider Certificate Program
- Stretchlab — Flexologist Training Program (FTP)
The CDC offers another quality training standard for the public health workforce. While their standard is not an internationally recognized standard developed by an ANSI approved SDO, it highlights and validates eight of the key components that lead to higher quality in education.6 CDC TRAIN is the Learning Management System for CDC courses, where 600+ courses currently meet these requirements.7

Is saving time on education and training important in the cleaning industry?
Absolutely!
The cleaning industry has long understood the value of education and training of frontline staff. From more efficient workflow, to reduced risk of injuries, education and training is a critical component of a competent and thriving organization. With current staffing shortages, turnover, and expectations for cleaning operations at an all-time high however, the need to education and train has never been so clear.
But we also know that there is room for improvement in cleaning education and training. In a recent survey, CloroxPro asked facility managers to describe their current training programs. Less than half said that their current programs are helpful (47%), easy to understand (46%) or are high-quality (32%)!8 In other words, current offerings are not meeting the needs of our industry and we are therefore wasting time.

In summary, CloroxPro launched the FIRST AND ONLY industry-wide training 3rd party accredited certificate course for commercial cleaners. They did this because they recognized that high-quality education and training was needed in the cleaning industry, and that a 3rd party accreditation against a standard was the best way to ensure that learning outcomes are achieved. Given the many challenges that the cleaning industry faces today, we can no longer afford to waste time on low quality education. As the new year approaches, consider offering an accredited course to save time on training employees, and help your organization thrive for years to come!
If you would like to learn more about or sign up for the CloroxPro™ HealthyClean™ Trained Specialist course, click here.
If you would like to read more about finding the right education and training program, click here:
References
1. ANSI National Accreditation Board. Certificate Accreditation Program [Internet]. [cited 2022 Dec 10]. Available from: https://anab.ansi.org/credentialing/certificate-issuers/
2. ASTM E2659-19 Standard Practice for Certificate Programs, 2018 [Internet]. [cited 2022 Dec 12]. Available from: https://webstore.ansi.org/standards/astm/astme265918?gclid=Cj0KCQiA4uCcBhDdARIsAH5jyUk5I4U8NtsLqh18RT61yDaKRLQ6qDC8-rY6Ub9sKUSZsKK0HKuEBHcaAjOSEALw_wcB
3. ANSI National Accreditation Board. Certificate Accreditation Program (Accredited) Directory [Internet]. [cited 2022 Dec 10]. Available from: https://anabpd.ansi.org/accreditation/credentialing/certificate-issuers/AllDirectoryListing?prgID=212,238&statusID=4
4. ICE 1100:2019 Standard – ACAP Standard for Assessment-Based Certificate Programs, 2019 [Internet]. [cited 2022 Dec 12]. Available from: https://my.credentialingexcellence.org/ice-product-details?id=07732e98-528e-eb11-8ced-dc98408f7f00
5. Institute for Credentialing Excellence. Accredited Program Search [Internet]. [cited 2022 Dec 10]. https://ice.learningbuilder.com/Public/MemberSearch/ProgramVerification
6. Centers for Disease Control and Prevention. Quality Training Standards [Internet]. [cited 2022 Dec 12]. https://www.cdc.gov/training/development/standards/index.html
7. CDC TRAIN. Welcome to CDC TRAIN [Internet]. [cited 2022 Dec 12]. https://www.train.org/cdctrain/welcome
8. CloroxPro Professional Online Facility Manager/BSC Study, October 2021: https://www.cloroxpro.com/resource-center/healthyclean-program-infographic/
There have been many exciting "aha" moments in my 18 years at Clorox. For example, I distinctly remember the excitement I felt when I learned about the difference between a sanitizer and a disinfectant. It seems silly to say now, but I called home to share something that even my mom, a diehard Clorox bleach user, didn’t know.
Another of these moments happed when I learned about risk assessments. At first, I liked that there was an established method for thinking through risks and how to reduce them…but my excitement grew significantly when I realized how risk assessments can be applied to everyday life! COVID-19 is a real-world example of a situation where a hazard (SARS-CoV-2) was identified along with what could be done to reduce risk (e.g. increasing ventilation, wearing masks, physical distancing, and vaccination).
In the cleaning industry, risk assessments and risk reduction also play a key role to ensuring the safety of frontline cleaners. Janitors and cleaners consistently have high rates of injuries and illnesses that lead to days away from work, so understanding how to do a risk assessment and reduce risk is vital.1,2
Here I break down the process into five easy steps:
Step 1: Understand the definitions
- A hazard is any source of potential damage, harm or adverse health effects on something or someone.3
- A risk, on the other hand, is the chance or probability that a person will be harmed or experience an adverse health effect if exposed to a hazard. It may also apply to situations with property or equipment loss, or harmful effects on the environment.3
- A risk assessment is the overall process used to identify hazards that have the potential to cause harm and evaluate their risk based on potential exposure to those hazards.4
- Risk Reduction are the things that are done to reduce the amount of risk or harm.
Step 2: Identify the hazards
Hazards fall into three main categories5:
- Biological include things like germs, mold, and insects or pests.
- Chemical include things like cleaning products and asbestos.
- Physical include things like slips, trips and falls and faulty or poorly designed tools and equipment.
Step 3: Identify the risks
Next assign a “level of risk” to each hazard based on the expected exposure for employees and what type of injury or illness could result from those exposures. In other words, risk is based on the likelihood that an exposure will occur as well and the expected outcome because of the exposure. For example, any hazard that could result in death or is irreversible and would be something that an employee would be commonly exposed to, would be considered a high risk. Risks are often identified as high, medium, and low.
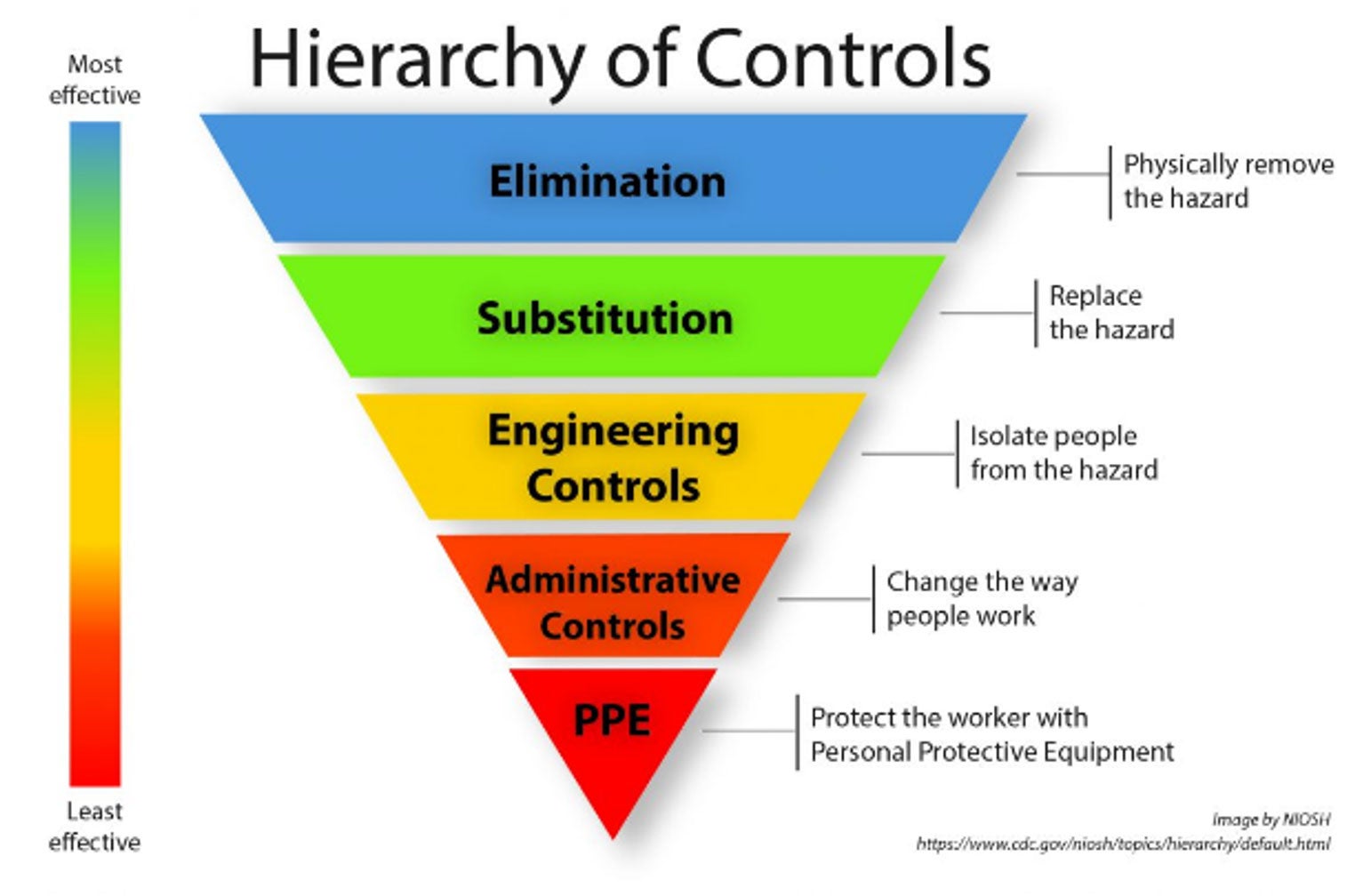
Step 4: Apply OSHA’s Hierarchy of Controls
In the workplace, once the risk assessment is complete, OSHA suggests using the hierarchy of controls to reduce the risk of any hazard where there is a chance of injury or illness. The hierarchy of controls is a tool that can be used to determine what actions to take. Starting at the top, it is always best to eliminate the hazard if possible. If that isn’t possible, then substitution is the next best option. From there, engineering controls, administrative controls, and PPE should be considered.6,7 Note that education and training help to reduce risk for frontline cleaners and should be part of every operation’s risk reduction strategy.
Here is an example of what this could look like for a cleaning operation:
| Hazard Type | Hazard | Risk of Injury or Illness (because of expected exposure) | Risk Reduction |
|---|---|---|---|
| Biological | Germs spread in the air (droplet): (e.g., Cold, Flu, Covid) | Infectious respiratory illness: Medium | • Increase air filtration • Wear mask • Consistently and properly clean and disinfect high touch surfaces |
| Germs spread on surfaces: (e.g., Staph, Norovirus) | • Skin infections • Infectious vomiting and/or diarrhea: Medium |
• Consistently and properly clean and disinfect high-touch surfaces • Select disinfectants with kill claims for germs of concern • Wear gloves |
|
| Bloodborne pathogens (e.g., HIV, HBV) | Bloodborne infections: High | • Wear gloves (at minimum) • HBV vaccination |
|
| Chemical | Corrosive disinfectant (EPA Cat I) | Chemical burns on skin and eyes: High | • Follow Directions for use • Wear appropriate PPE • Swap out product for one that does not require the use of PPE (EPA Cat III & IV) |
| Physical | Heavy upright vacuum | Musculoskeletal injury: High | Swap out for backpack vacuum |
| Repetitive motion when mopping large spaces | Repetitive motion injury: High | • Use microfiber mop head over cotton mop • Purchase auto floor scrubber |
“Education and training help to reduce risk for frontline cleaners and should be part of every operation’s risk reduction strategy. “
Step 5: Combine the results, write down the plan, and act!
As a final step, look across the results and develop a plan. Consider all risk reduction measures. In some cases, a step to reduce risk is needed for one hazard, but not for another. For example, when it comes to wearing gloves, even when not needed to prevent exposure to the product itself, they should be worn to protect frontline cleaners from exposure to germs and other hazards while doing cleaning and disinfecting tasks.
“When it comes to wearing gloves, even when not needed to prevent exposure to the product itself, they should be worn to protect frontline cleaners from exposure to germs and other hazards while doing cleaning and disinfecting tasks.“
Write down the plan and act by clearly communicating the outcomes to employees. This will ensure they know what the job entails, what you are doing to reduce risks, and what they are expected to do as well. To help manage any next steps that are not immediately actionable, address those with the highest risk first. An added benefit of writing things down is that it will help meet OSHA’s requirements. Revisit your facilities risk assessment on an annual basis and when things change.
What other “aha” moments would you like to her about? Reach out at lori.strazdas@clorox.com and let me know!
References
1. U.S. Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days away from Work, 2015 [Internet]. News Release [cited 2022 Sept 10]. Available from: https://www.bls.gov/news.release/pdf/osh2.pdf
2. U.S. Bureau of Labor Statistics. Occupation Snapshot Janitors and cleaners, 2015-2019 [Internet]. Injuries, Illnesses, and Fatalities. [cited 2022 Sept 10]. Available from: https://www.bls.gov/iif/oshwc/case/osn-janitors-2015-19.htm
3. Canadian Centre for Occupational Health and Safety. Hazard and Risk [Internet]. OSH Answers Fact Sheets [cited 2022 Sept 14]. Available from: https://www.ccohs.ca/oshanswers/hsprograms/hazard_risk.html
4. Canadian Centre for Occupational Health and Safety. Risk Assessment [Internet]. OSH Answers Fact Sheets [cited 2022 Sept 14]. Available from: https://www.ccohs.ca/oshanswers/hsprograms/risk_assessment.html#:~:text=Risk%20assessment%20is%20a%20term,analysis%2C%20and%20risk%20evaluation
5. Gislason E. National Association of Safety Professionals. Dec 2018 Newsletter [Internet]. Types of Hazards [cited 2022 Sept 9]: Available from: https://naspweb.com/blog/types-of-hazards/
6. Health and Safety Executive. Risk Assessment [Internet]. Managing risk and risk assessments at work [cited 2022 Sept 10] Available from: https://www.hse.gov.uk/simple-health-safety/risk/index.htm

A new employee just joined our team. Multiple team meetings were scheduled so we could get to know her. She was given a new computer and a smartphone, both preloaded with useful software and tools to help her do her job. She was also provided with a three-page onboarding plan, that included multiple training courses, to help her get up to speed quickly.
Why did we do all this?
We did it because we know that these things are important for engagement, and if she is engaged, she will want to stay with our company for a while.1 With the “great resignation” among us, our effort is more critically important than ever as turnover costs money and reduces efficiency. In this blog I will use our new team members experience to highlight three simple ways that cleaning managers can help increase employee engagement and reduce the cost of turnover in their organizations.
Get to know and use their superpowers
“What is your superpower?” is one of the most common questions asked of our new employees. Superpowers go beyond skills that have been or can be learned, like using Microsoft Excel spreadsheets, or knowing the steps to take to safely cleanup blood from a surface. Instead, they are the things that someone is inherently good at doing and that they can do with minimal effort.2 Some examples of superpowers are staying calm in stressful situations, being sensitive to what others are thinking and feeling, and collaborating well with others even when they have different views. The importance of recognizing superpowers is that they help employees feel seen and valued. This can help make them want to stay with an organization, but there is even more power in them than that. Superpowers can also help organizations operate more productively and efficiently. For example, if there is someone on the team who is good at and enjoys organizing events, they may be willing to be put in charge of team building activities. This is a win-win situation for a manager, who can then focus on other tasks. Invest time in learning as much as you can about your employees and watch engagement grow and turnover disappear.
Supply them with the best tools, equipment, and products
Everyone likes to use the best stuff. When it comes to tools, equipment, and products, there is a range in quality. To help front line cleaners do their jobs more efficiently, effectively, and safely, supply them the best you can afford (while setting the expectation that they need to be well cared for, so they last a long time). For example, here are a few options to consider:
- Microfiber cloths provide superior soil collection and removal over regular cotton cloths, and lead to noticeably cleaner environments.3
- Ready-to-use products cut out product preparation time and reduce the chance that a prepared product will be overdiluted (efficacy concerns), under diluted (toxicity concerns), or in a mislabeled secondary container (OSHA compliance concerns).
- Electrostatic sprayers provide a faster and more ergonomic solution to traditional manual trigger sprayers.4
- Specialty products that focus on specific needs can help get jobs done faster and with less effort.
- “Robots”, like automatic floor cleaners, can save considerable time, labor, and even reduce the risk of injury.
An operation that chooses the best products, tools, and equipment over one that does not will win an employee’s heart every time, which will lead to better engagement and less turnover.
Provide high-quality education & training
As in any field, front-line cleaners also need education and training to do their jobs efficiently, effectively, and safely. Education and training should include making sure that employees understand why their job is important, what policies and procedures they need to follow, and how to use tools, equipment, and products. Ongoing education and training also have the benefit of informally communicating that change is normal and should expected. There are many options for education and training for front-line cleaning staff and just like tools and equipment, they range in quality. To help you find or create the most efficient, effective, and valuable education and training programs, check out these blogs I wrote on Instructional Design, The ABC of Credentialing, and The Cs of Credibility. When education and training are provided, employees will better understand the value of the work they do, be better at doing their jobs, and be more open to change. These incredible outcomes are all common in engaged employees and will help them stay with your organization.5
We are in a challenging time right now with staffing shortages and increased customer demands for clean and safe indoor environments. Taking a lead from our organization, recognize your employees as individuals and use their superpowers to help the team, provide them with the best tools, equipment, and products so they can do their jobs efficiently, effectively, safely, and even enjoy using the latest and greatest technology. Finally, invest in their education and training so they understand why their jobs are important, become competent in their roles, and expect change. These are three simple ways to increase engagement and reduce turnover, so you get back to the most important task at hand: creating healthier and safer shared spaces for people to work, learn, live, and thrive.
References:
- Sorenson S. How Employee Engagement Drives Growth. [Internet] Gallup Workplace. [cited 2022 June 13] Available from: https://www.gallup.com/workplace/236927/employee-engagement-drives-growth.aspx
- Henley D. Discover your superpower at work. Forbes [Internet]. 2021 [cited 2022 June 10]; Available from: https://www.forbes.com/sites/dedehenley/2021/03/07/discover-your-superpower-at-work/?sh=51acea2b7213
- Mollenkamp B. The right tool for the job. Cleanlink [Internet]. 2016 [cited 2022 June 10]; Available from: https://www.cleanlink.com/hs/article/Differences-Between-Microfiber-And-Cotton--20239
- Cadnum JL, Jencson AL, Livingston SH, Li D, Redmond SN, Pearlmutter B, et al. Evaluation of an Electrostatic Spray Disinfectant Technology for Rapid Decontamination of Portable Equipment and Large Open Areas in the Era of SARS-CoV-2. Am J Infect Control [Internet]. 2020 [cited 2022 June 10]; Available from: https://doi.org/10.1016/j.ajic.2020.06.002
- Bersin J. New Research Shows “Heavy Learners” More Confident, Successful, and Happy at Work [Internet]. LinkedIn. 2018 [cited 2022 June 10]. Available from: https://www.linkedin.com/pulse/want-happy-work-spend-time-learning-josh-bersin/

Want to make sure the program you are investing in is credible? I am sure you do, but with the sheer number of online education and training programs available today, how do you do that? Understanding what makes a program credible is essential to ensuring a return on your investment, and in today’s competitive and resource constrained climate, it is even more important than ever!1
Credible, by definition, means “offering reasonable grounds for being believed.”2 For education and training programs, you can look at these three C's: Content, Confirmation and Credentials.
In this blog, I will cover these three aspects of an education and training program that can help with assessing its credibility. If you are interested in learning more about finding the right education and training program, check out my previous two blogs: The ABC's of Credentialing and the Why Instructional Design Matters.
Content
The first question to ask is who developed the content and whether the person has the experience and expertise needed to teach the topic to someone in your position. Experience and expertise can be evaluated in a few different ways, but fortunately we are lucky today to have a great online resources, like LinkedIn, to help.
In addition, while content created by a single qualified individual can be appropriate, understanding if there were multiple experts involved in developing the course helps ensure that learning represents a broad point of view and not just the perspective one expert. A general rule of thumb is that the more qualified experts involved, and the more collaborative an effort, the more credible the program.
Confirmation
The next aspect to assess is whether the final evaluation (also called assessment, exam, test, or quiz) at the end of the program confirms that learning has occurred. While this may seem like somewhat of a “no brainer” (all tests and quizzes assess learning right?), not all evaluations are created equal.
How does one assess the assessment? You can start by finding out what the learning objectives are for the course and how many questions are on the final evaluation. There should be at least one, but in most cases more, questions for each learning objective. This explains why some of the tests you took in school were so long! Schools need to confirm that students learn the curriculum and there is no way to do it with short tests. The same holds true in adult education. The bottom line here is that if you are considering taking a three hour course, you should expect to learn a lot from it. And to confirm that you did, you should, at the very least, expect there to be a robust exam.
Credentials
Lastly, consider these questions:
- How can you tell if someone’s credential is valid
- What are the measures taken to protect the validity of the credential earned?
This is another aspect of education and training that is built in to high quality programs, like those that are accredited. While it may take a lot of work to obtain a credential, in reality, anyone can say they have earned a credential or even provide “proof” of it by copying and altering another person’s certificate. The more credible programs will offer ways to make sure that the value of a credential is protected. This includes a verifiable link on the certificate in the form of a QR code and/or by providing a digital badge instead of just a static logo. Digital badges provide metadata that can verify that the credential is valid. These verification steps allow for stakeholders to confirm who a credential belongs to and if it is current. This can be helpful in a number of situations, including when an employer is evaluating a new potential employee.
This concludes my three part series on finding the right education and training program. With labor shortages, buildings reopening, and an increasing demand for cleaning for health, training and education of staff is more important than ever.3 Are you ready to take action and a find a program that is right for you? If yes, here is a summary list of the questions to ask. Happy learning!
- Is it a certificate or certification?
- Is it third party accredited?
- Was the course instructionally designed?
- Who developed the content?
- Is the exam robust enough to confirm that learning occurred?
- What is the credential and is it protected?
References
1. Federal Trade Commission. Choosing a vocational school or certificate program [Internet]. FTC Consumer Advice. [cited 2022 March 15]. Available from: https://consumer.ftc.gov/articles/choosing-vocational-school-or-certificate-program
2. Merriam-Webster. Definition of Credible [Internet]. Merriam-Webster. [cited 2022 March 15]. Available from: https://www.merriam-webster.com/dictionary/credible
3. Amy W. Richardson. 2022 CMM In-House/Facility Management Benchmarking Survey Report [Internet]. CMM Online. [cited 2022 March 20]. Available from: https://www.cmmonline.com/articles/fmsurvey2022?_ga=2.193544229.920623462.1648472434-1882373344.1633539137

Sometimes it’s hard to remember that germs existed before COVID-19. I assure you they did, but the truth is the pandemic has become a catalyst in all our lives that sparked an immediate reverence and awareness about the importance of cleaning for health. With that came an acute mindfulness of the critical role that commercial cleaners play in helping to prevent the spread of germs in shared and public spaces.
From the start of the outbreak, commercial cleaning professionals have been thrust into the spotlight and classified as frontline essential workers. With a new emphasis on safeguarding public health, the bar for what was considered “clean” was raised, and many habitual cleaning practices were no longer enough. However, many cleaning professionals remain unsure what this means they should do differently and, importantly, how to do this efficiently and safely.
Cleaning and disinfecting beyond the pandemic
Research shows that heightened consumer interest and demand for maintaining cleaning and disinfecting routines in public spaces, continues to be top of mind. In fact, 60% of Americans bring disinfectants with them regularly to disinfect high-touch surfaces outside of the home.1 Rightfully so, because there are many other germs beyond COVID-19 that commonly spread via surfaces — such as cold and flu viruses, norovirus and MRSA. Outbreaks caused by these germs aren’t new and can disrupt, or even shut down, schools and other facilities that communities rely on every day. As a result, cleaning for health will remain a key part of a holistic strategy to help reduce this risk.
The pandemic highlighted the need for a more balanced approach to disinfection that can be sustained long-term. CloroxPro refers to this approach as Smart Disinfection, which, as its name suggests, emphasizes that there is a time to clean and a time to disinfect.
Smart Disinfection means targeting “higher-risk surfaces” and “higher-risk areas” to help reduce the transmission of germs that can cause illness, including increased occasions where populations are more vulnerable to infections such as daycares, schools, and eldercare and healthcare facilities.
CloroxPro is innovating for the cleaning professional
In a recent survey of facility managers and buildings service contractors, 91% say the staff at their company or facility have had to learn new cleaning and disinfecting protocols, and 96% say that janitorial staff are asked to do more now to help provide greater confidence to occupants and visitors.2 But training programs have not kept up with the needs of the industry.
To make this type of knowledge and education accessible, CloroxPro has developed CloroxPro™ HealthyClean™, a new online learning platform that delivers best-in-class education and training to help ensure cleaning professionals get the knowledge and skills needed to clean for health effectively, efficiently and safely. HealthyClean offers the only industrywide certificate course designed for the commercial cleaning industry to be accredited by the American National Standards Institute National Accreditation Board. The training covers actions that can be taken to do the job safely and effectively, the science behind how germs spread, and provides easy-to-follow procedures and best practices to ensure facilities can be cleaned and disinfected in a way that is efficient and sustainable long-term.
Discover more at CloroxPro.com/HealthyClean.
References
1. Clorox Custom Research, Clean Confidence Index: Wave 2 (n=2000), February 2021
2. Clorox Professional Online Facility Manager/Builder Service Contractor Study, October 2021