What’s Causing Healthcare-Associated Infections (HAIs)? Key Takeaways from the New NHSN Data on Antimicrobial-Resistant Pathogens Associated with Adult HAIs.
Hot off the press is the Centers for Disease Control and Prevention’s (CDC’s) new biennial summary of data submitted to the National Healthcare Safety Network (NHSN) on antibiotic-resistant organisms (AROs) causing HAIs. This fourth summary covers the period 2015–2017 and like previous reports, includes data on central-line associated bloodstream infection (CLABSI), catheter-associated infection (CAUTI), surgical site infection (SSI) and ventilator-assisted event (VAE) submitted by over 5,600 healthcare facilities. Data on C. difficile infections is not included.
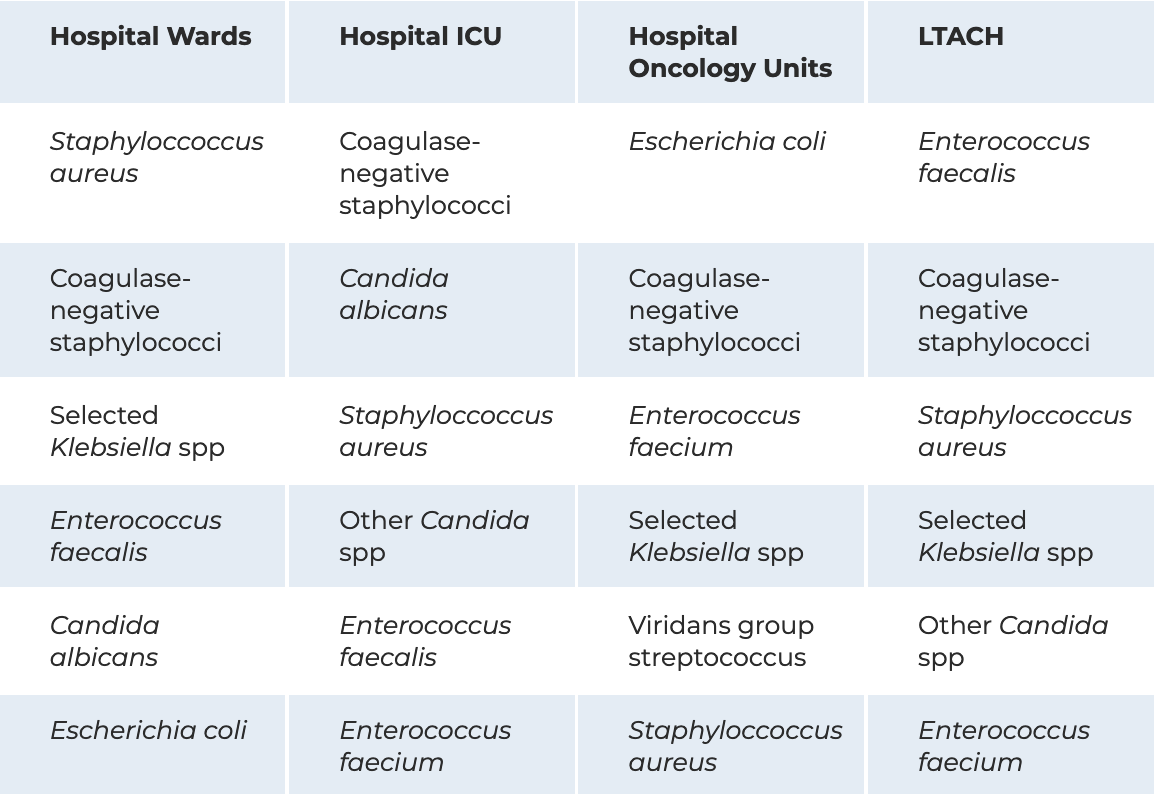
However, thanks to the expansion of Centers for Medicare and Medicaid Services (CMS) reporting on HAIs, the report also provides additional data stratified by infection type, facility type and sizes, surgery type, and location — hospital ward, intensive care unit, oncology unit, long-term acute care hospital (LTACH) and in-patient rehab facility — as well as data on antimicrobial susceptibility.

Highlights (and Lowlights) From the Report
There’s a lot of detailed information in the open-access article published in Infection Control and Hospital Epidemiology but it’s well organized with many easy-to-read tables to guide the reader to topics of specific interest.
Here are some key pieces of information that jumped out to me, which may be useful when thinking about infection prevention activities and strategies in hospitals: The rank order for the four HAI types reported was SSI (43%) CAUTI (30%), CLABSI (25%), PVAP (possible ventilator-assisted pneumonia) (3%).
- The report lists the top 15 pathogens causing any of the four HAIs, with the top five pathogens being, in decreasing order, Escherichia coli (18%), Staphylococcus aureus (12%), selected Klebsiella spp. (9%), Pseudomonas aeruginosa (8.0%) and Enterococcus faecalis (8%). This is almost the same as 2012-2014, the difference being that P. aeruginosa switches places with coagulase-negative staphylococci.
- Oncology units have a different distribution of pathogens than other units. In particular, a new group of pathogens, appearing at number 13 is viridans group streptococci, which caused almost 9% of CLABSIs reported in oncology units.
- The frequency of pathogens causing CLABSI differs considerably between hospital units as seen by the table below showing the top 6 pathogens causing CLABSI. The differences are less pronounced for CAUTI. One important point to note is that when grouped at the genus level, Candida spp. were the most common CLABSI pathogen in hospital wards/ICU, making up 25% of ICU pathogens.
Six Most Frequently Reported Adult CLABSI Pathogens By Location (2015–2017)
- The proportion of pathogens causing HAIs in LTACH that were non-susceptible to antibiotics was higher compared to other locations, reflecting the well-established heightened antimicrobial resistance found in these facilities. In a similar vein, device-associated HAIs – CLABSI, CAUTI and VAE had significantly higher proportions of non-susceptible pathogens as compared to SSI
- Some good news is that the percentage of Candida isolates that are susceptible to fluconzazole has increased over time; susceptibility testing has been recommended since 2016 and in the future, CDC hopes to be able to track a national resistance metric for Candida spp.
This expanded report with additional hospital locations and antimicrobial susceptibility data builds on previous reports to provide a more comprehensive picture of the burden of HAIs in the US, and the challenges of antimicrobial resistance. Regular review of pathogen and antimicrobial resistance data for all units, but particularly those at highest risk such as ICUs, oncology and transplant units can also guide infection prevention strategy.
Environmental Disinfection Is a Critical Strategy for HAI Prevention
As I read through this, a few useful actions around environmental cleaning and disinfection that came to mind included:
- Checking disinfectants used in your facility to check that they have EPA-approved claims against the top HAI-causing pathogens
- Making sure that appropriately effective disinfectants are used in hospital units, particularly high-risk units
- Ensuring that all staff are aware of the correct contact times for target pathogens and follow the product directions for use.
The comprehensive findings of this report certainly provide plenty to mull on, and while I’ve offered some key takeaways above, I encourage all infection prevention professionals to take a read for themselves.
Citation: Weiner-Lastinger LM, Abner S, Edwards JR, Kallen AJ, Karlsson M et al. Antimicrobial-resistant pathogens associated with adult healthcare-associated infections: Summary of data reported to the National Healthcare Safety Network, 2015-2017. Infect Control Hosp Epidemiol. 2019 Nov 25:1-18. doi: 10.1017/ice.2019.296. [Epub ahead of print]


